A Comparative Dosimetric Evaluation in Carcinoma Right Breast for Convex Chest Wall, Post Breast Conservation Surgery using two Distinct Radiotherapy Techniques
Harpreet Kaur, Sangeeta Hazarika, Jefy Ninan, Ajay Khatri, Prasobh C, Pooja Handa, Kamal Verma, Sandeep Goel and Subodh Pande
Harpreet Kaur1*, Sangeeta Hazarika1, Jefy Ninan1, Ajay Khatri2, Prasobh C1, Pooja Handa1, Kamal Verma1, Sandeep Goel1 and Subodh Pande1
1Department of Radiation Oncology, Artemis Hospitals, Gurugram, India
2Department of Radiation Oncology, Narayana Hospitals, Gurugram, India
- *Corresponding Author:
- Harpreet Kaur
Department of Radiation Oncology
Artemis Hospitals, Sector 51
Gurugram, India
Tel: +917065688139
E-mail: harpreetsaini111@ ymail.com
Received Date: October 27, 2020; Accepted Date: November 11, 2020; Published Date: November 18, 2020
Citation: Kaur H, Hazarika S, Ninan J, Khatri A, Prasobh C, et al. (2020) A Comparative Dosimetric Evaluation in Carcinoma Right Breast for Convex Chest Wall, Post Breast Conservation Surgery Using Two Distinct Radiotherapy Techniques. Insights Med Phys Vol: 5 No: 3:12
Abstract
Background and purposes: The aim of this research was to compare a six-beam Dynamic Multi Leaf Collimator (DMLC) technique with a restricted Tangential Volumetric Modulate Arc Therapy (tVMAT) technique for convex chest wall after Breast-Conserving Surgery (BCS).
Materials and methods: Twenty patients with carcinoma right-breast whose chest walls were convex or barrel shaped (curvature distance equal to or more than 3 cm) were selected for this study. All the patients were already treated with breast conserving surgery. Patients were prescribed 45 Gy in 25 fractions followed by boost to the tumor bed. They were planned using two different techniques including: 1) Six beam DMLC; and 2) Tangential Volumetric Arc Therapy (tVMAT). All other normal tissues and OAR including ipsilateral lung, contralateral lung, contralateral breast, heart, spinal cord, thyroid, liver and esophagus were contoured according to the RTOG guidelines. The planned volumetric dose of PTV and OARs were compared and analyzed.
Results: Hetrogeneity Index (HI) and Conformity Index (CI) were comparable for both tVMAT and DMLC. PTV volume receiving 95% of prescription dose was better in DMLC (96.41 ± 1.03) as compared to tVMAT (92.24 ± 13.31). V100% was much better in DMLC (83.91 ± 3.25) as compared to tVMAT (70.18 ± 9.74). V107% was reduced in tVMAT (1.93 ± 3.39) than DMLC (2.59 ± 5.08). D95 (Gy) was better in DMLC (96.41 ± 1.03) than tVMAT (92.24 ± 13.31). For ipsilateral lung, V10 and V5 were greatly reduced in DMLC (36.77 ± 2.31, 47.61 ± 2.84) but for tVMAT, V10 was more than the limits (43.95 ± 10.15) but V5 was well within the limit (56.94 ± 18.37). The V20, V30 and mean ipsilateral lung dose was less in DMLC. Mean heart doses in DMLC and tVMAT were 2.61 ± 0.94 and 4.57 ± 2.61. D0.03 of heart was much better in DMLC (24.72±10.70) as compared to tVMAT (32.38 ± 9.65). Mean contralateral breast dose was better in DMLC (2.39 ± 1.28) as compared to tVMAT (4.07 ± 1.70). All other OARs like contralateral lung, Esophagus, Spine, Thyroid and Liver were slightly better in DMLC as compared to tVMAT. Volume of 50% isodose line (3409.63 cc) as well as 20% isodose line (4296.85) was greatly reduced in DMLC as compared to VMAT (3626.70 versus 4750.48 respectively). Total number of monitor units required for delivering both the treatment plans were comparable.
Conclusion: Six beam DMLC treatment planning techniques are best suited for BCS patients with a more convex chest wall. The VMAT plans are more conformal and their treatment time was less but with DMLC technique, various OAR doses and integral dose to normal tissue were less. Similar technique can be applied to Left BCS cases as well.
Keywords
Dosimetry; Chemotherapy; Radiotherapy; Isodose line; Dose heterogeneity
Abbreviations
DMLC: Dynamic Multi Leaf Collimator; tVMAT: Tangential Volumetric Modulate Arc Therapy; BCS: Breast-Conserving Surgery; HI: Heterogeneity Index; CI: Conformity Index
Introduction
Breast-Conserving Surgery (BCS) followed by adjuvant radiation therapy is an efficacious organ-preserving alternative treatment to mastectomy for women with early-stage breast cancer [1,2]. Randomized trials have shown that the BCS is equivalent to mastectomy in terms of survival. During radiotherapy, size and shape of irradiated breast highly influences the dose homogeneity and effects of treatment [3]. Recent advancements in technology and radiotherapy delivery techniques have led to improved dose distribution and increased efficiency of treatment. Many studies have been reported on comparing the distribution of dose for breast cancer radiotherapy techniques [4-8].
However there are various techniques being introduced till now which show lesser OAR doses [9-11]. Volume Metric Arc Therapy (VMAT) is a well-known technique that uses rotating gantry during dose delivery [10]. Nevertheless, it is well recognized that VMAT reduces the treatment time [12] but raises the volume of lower doses. In the previous dosimetric studies full or continuous partial arcs have been used in VMAT treatment planning [13,14]. But in this situation additionally dose to contralateral lung, opposite breast, heart can be high. While considering breast radiotherapy one must consider lower dose to numerous OARs. Lamentably, a variety of sufferers expand radiation induced inclusive of breast fibrosis, modifications in the breast appearance and overdue pulmonary and cardiovascular complications [15-17]. Simultaneously, to avoid radiation prompted pulmonary complications, dose volume constraints for ipsilateral lung must additionally be employed [16].
One of kind studies has been carried out for small volume breast instances [10-12] but this is novel study that includes patients having convex breast or barrel shaped breasts. Previously we have done one study with tangential Volumetric Arc Therapy (tVMAT) by using 30 degree arcs [18] at different centre but due to convex shape of chest wall 30 degree arc was not enough to cover the PTV. Despite the fact that plans were being attempted without giving any constraints to OARs but still coverage of PTV was not adequate due to saturation of plans.
Our DMLC plans were alternative option of tVMAT where 6 different angled beams were used. Along with this tangential VMAT arc angles were also increased so that both the techniques should be comparable on various PTV and OAR parameters.
Materials and Methods
Patient selection
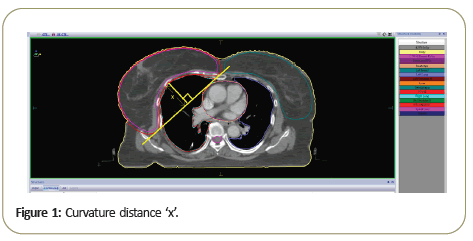
The study included retrospective analysis of Dose Volume Histogram (DVH) parameters for 20 patients aged (50 ± 6.2) with right sided breast cases treated with adjuvant radiotherapy following Breast Conservative Surgery (BCS) and chemotherapy (if indicated). The selection criteria for patients were based upon the curvature of patient breast (Figure 1). Curvature distance ‘x’ found by drawing a straight line joining the medial and lateral edges of the PTV and further putting a perpendicular bisector from lower middle border of ribs PTV (Figure 1). If this distance was equal to or more than 3 cm that particular patient was taken for this study. The issue with highly convex shaped chest is that the small tVMAT arc angles are not ideal for them. For covering the PTV borders on medial and lateral side more jaw opening is required which will lead to more OAR doses.
Simulation and structure delineation
The Patients were positioned supine on All-In-One board (AIO) with both arms in fully abducted position. The patients were simulated with CT simulator (Philips Medical Systems) in treatment position immobilized with the Orfit Cast. Three external radiopaque fiducial markers placed on the cast were used for laser re-positioning and reproduction; CT images were acquired with 3 mm slice thickness from the angle of mandible till the lower border of L4 vertebra. Acquired images were contoured using Monaco contouring station. The Clinical Target Volume Breast (CTVbreast) was contoured according to RTOG 3509 which included cranial-clinical reference plus second rib insertion, caudal-clinical reference plus loss of CT apparent breast, anterior-skin, posterior-excludes pectoralis muscles, chestwall muscles, ribs/Includes pectoralis muscles, chestwall muscles, ribs, lateral- clinical reference plus mid axillary line typically excludes latissimus, medial-sternal rib junction. The Clinical Target Volume (CTVboost) for the tumor bed was defined as lumpectomy cavity which was planned for concomitant boost by electron or photon depending on the depth of the lumpectomy cavity. PTVbreast with margin of 5 mm to CTVbreast was contoured which was further clipped 2 mm from the patient skin. Similarly PTVboost was drawn with 5 mm margin to CTVboost. All other normal tissues and OAR including ipsilateral lung, contralateral lung, contralateral breast, heart, spinal cord, thyroid, liver and esophagus were contoured according to the RTOG guidelines. All the Patients were planned using Monaco (5.11.02) (Elekta CMS, Sunnyvale CA) Planning station with Dynamic Multi Leaf Collimator (DMLC) and Volumetric Modulated Arc Therapy (VMAT).
Treatment technique
The treatment was delivered using Infinity Linear Accelerator with leaf width of 5 mm at isocentre. The patients were treated with a dose of 45 Gy delivered in 25 fractions by 6 MV photons. Thereafter, a boost of 15 Gy in 6 fractions was delivered with electron or photons to the lumpectomy site.
Infinity is equipped with integrated digital control of leaves with dynamic leaf guides. Accurate leaf positioning was controlled by Rubicon optical technology. Inverse planning was done utilizing Monte Carlo semi-biological algorithm with grid size of 3 mm. All the sequencing parameters, minimum segment width, maximum control points, fluence smoothing, statistical uncertainty per plan were kept same for both DMLC and VMAT. Auto flash margin of 1.5 cm was given beyond the surface of the skin to extend the fluence outside the body contour.
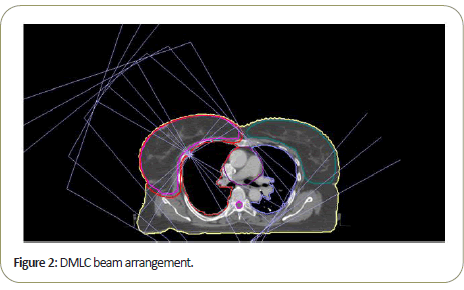
Beam arrangements for both planning techniques are depicted in Figures 2 and 3. For DMLC planning, 6 coplanar tangential beams with gantry angles 60°, 50°, 40° and 210°, 220°, 230° were selected. Number of control points for each beam was kept 80. The DMLC treatment plans were delivered through a sliding window MLC. The treatment delivery time (excluding setup time) was recorded but that does not include time required to rotate from one gantry angle to another. To reduce the manual work of rotating gantry composite fields were given.
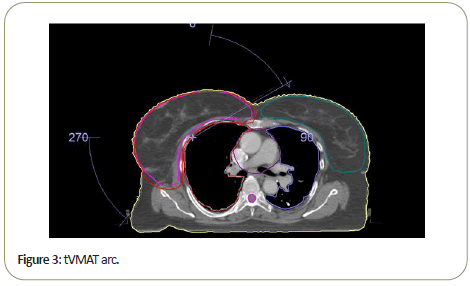
For tVMAT planning, two coplanar tangential arcs of 50° were selected. Gantry angles were decided to be 60° and 250°. Arc rotations were kept in counter clock wise direction. Arc angle of left anterior oblique arc was selected in such a way that it should avoid direct entrance in ipsilateral lung as well the contralateral breast simultaneously. Arc increment was kept at 30° in all the plans. Throughout the treatment plan system optimization, the continuous gantry motion was modelled as a number of control points, which included the treatment parameters such as MLC aperture shaping, the speed of gantry, and the dose rate. Between the two control points, the change of the parameters and MLC positions was linear.
The main criteria for both DMLC and tVMAT was to achieve at least 95% of the prescribed dose to cover at least 95% of PTV volume while minimizing the dose to the normal tissues. In both the plans collimator angles were set to zero. Plans were approved once it was found satisfactory with respect to coverage of PTV and avoidance of organ at risk according to our institutional criteria. Attempts were made to keep both the plans comparable in coverage, conformity and heterogeneity. DVHs were used for evaluation of dose to OARs.
Parameters for statistical evaluation of plans
Dose- volume histograms were generated for the PTVs and all OAR for dose analysis. The Heterogeneity Index (HI) was measured by D5%-D95%. Following parameters were recorded for each plan: PTV minimum dose (Dmin), PTV mean dose (Dmean), PTV maximum dose(Dmax), Dose received by 95% of the PTV volume(D95%), Volume receiving 95% of the prescribed dose (V95%), Volume receiving 100% of the prescribed dose (V100%), Volume receiving 107% of the prescribed dose (V107%), Conformity Index (CI), Heterogeneity Index (HI); heart mean dose, volume of heart receiving 25% of the prescription dose(V25) and dose received by 0.03 cc (D0.03), the percentage of volume of heart receiving a dose of 25 Gy (V25 ); ipsilateral lung mean dose and the percentage of volume of ipsilateral lung receiving a dose of 5 Gy (V5), 10 Gy (V10), 20 Gy (V20), 30 Gy (V30), and maximum dose (Dmax); contralateral lung: mean dose and the percentage of volume of contralateral lung receiving 5 Gy (V5); mean dose and maximum dose for contralateral breast; mean dose and maximum dose to liver; mean dose to thyroid and esophagus; maximum dose to spine; Volume of body receiving 50% of prescription dose and volume of body receiving 20% of prescription dose. The number of MUs, treatment time, MU efficiency and time taken for optimization were also recorded for analysis.
Results and Discussion
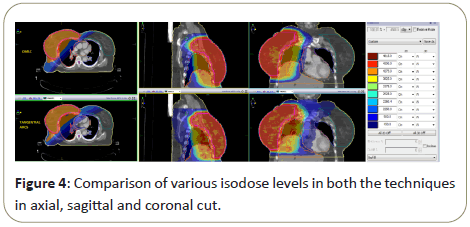
A comparison of dose distributions for a right breast cancer patient between (a) DMLC and (b) Tangential VMAT on axial, sagittal, and coronal planes is shown in Figure 4. PTV45 is shown in thick red colour with its isodose colour wash ranging from 5500 cGy down to 500 cGy are also depicted. Organs at risk (OARs) including ipsilateral (right) lung, contralateral (left) lung, contralateral (left) breast and heart with its isodose colour wash ranging from 4815 cGy down to 450 cGy are also shown.
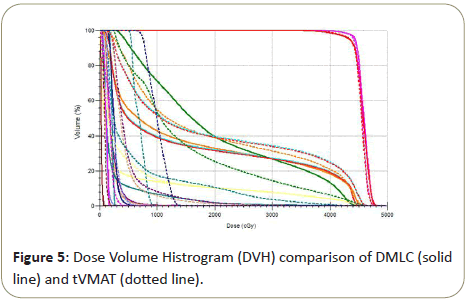
Dose Volume Histogram comparison of both the techniques is shown in Figure 5 where dotted line is for tVMAT and solid line represents DVH for DMLC.
Dosimetric comparison of tVMAT plans and DMLC in tabular form is shown in Table 1 with mean and standard deviation values for the PTV, heart, ipsilateral lung, contralateral lung, and contralateral breast. Heterogeneity Index (HI) and Conformity Index (CI) were comparable for both t VMAT and DMLC. PTV volume receiving 95% of prescription dose was better in DMLC (96.41 ± 1.03) as compared to tVMAT (92.24 ± 13.31). V100% was much better in DMLC (83.91 ± 3.25) as compared to tVMAT (70.18 ± 9.74). V107% was reduced in tVMAT (1.93 ± 3.39) than DMLC (2.59 ± 5.08). D95 (Gy) was better in DMLC (96.41 ± 1.03) than tVMAT (92.24 ± 13.31). All other parameters like Dmin, Dmax, Dmean, were comparable in both the plans.
| Tangential VMAT | DMLC | |
|---|---|---|
| PTV | ||
| Dmin(Gy) | 23.82 ± 3.24 | 23.28 ± 2.71 |
| Dmean(Gy) | 45.27 ± 0.39 | 45.68 ± 0.26 |
| Dmax(Gy) | 49.75 ± 0.60 | 49.72 ± 0.33 |
| D95(Gy) | 46.26 ± 13.02 | 43.63 ± 0.70 |
| V95 (%) | 92.24 ± 13.31 | 96.41 ± 1.03 |
| V100 (%) | 70.18 ± 9.74 | 83.91 ± 3.25 |
| V107 (%) | 1.93 ± 3.39 | 2.59 ± 5.08 |
| Conformity Index (CI) | 0.66 ± 0.09 | 0.76 ± 0.05 |
| Heterogeniety Index (HI) | 1.09 ± 0.01 | 1.09 ± 0.01 |
| Ipsilateral lung | ||
| V10 (%) | 43.95 ± 10.15 | 36.77 ± 2.31 |
| V20 (%) | 32.16 ± 11.94 | 28.78 ± 3.04 |
| V30 (%) | 26.46 ± 9.38 | 23.85 ± 5.25 |
| V5 (%) | 56.94 ± 18.37 | 47.61 ± 2.84 |
| Mean dose(Gy) | 16.48 ± 3.23 | 14.13 ± 1.21 |
| Heart | ||
| Mean dose(Gy) | 4.57 ± 2.61 | 2.61 ± 0.94 |
| V25 (%) | 1.17 ± 1.84 | 0.21 ± 0.40 |
| D0.03cc(Gy) | 32.38 ± 9.65 | 24.72 ± 10.70 |
| Opposite breast | ||
| Mean dose(Gy) | 4.07 ± 1.70 | 2.39 ± 1.28 |
| D0.03cc(Gy) | 37.05 ± 6.12 | 36.06 ± 10.65 |
| Contralateral lung | ||
| V10 (%) | 0 | 0 |
| V20 (%) | 0 | 0 |
| V30 (%) | 0 | 0 |
| V5 (%) | 0.35 ± 0.87 | 0.04 ± 0.15 |
| Mean dose (Gy) | 1.56 ± 0.52 | 1.17 ± 0.14 |
| Esophagus | ||
| Mean dose (Gy) | 2.54 ± 1.38 | 1.66 ± 0.30 |
| Spine | ||
| Maximum dose (Gy) | 2.61 ± 1.13 | 1.77 ± 0.26 |
| Thyroid | ||
| Mean dose (Gy) | 5.07 ± 3.01 | 2.86 ± 2.10 |
| Liver | ||
| Mean dose (Gy) | 8.51 ± 4.67 | 6.06 ± 2.42 |
| D0.03cc (Gy) | 46.48 ± 1.92 | 46.48 ± 1.89 |
| Volume of 50% Isodose line(cc) | 3626.7 | 3409.63 |
| Volume of 20% Isodose line(cc) | 4750.48 | 4296.85 |
| Total MUs | 711.81 | 710.23 |
| Treatment Time(sec) | 129.48 | 297.93 |
| Time taken for optimization (sec) | 798.97 | 929.95 |
| MU efficiency | 98.75 ± 3.26 | 98.67 ± 2.31 |
Table 1: Dosimetric comparison statistical data of tVMAT plans and DMLC in tabular form.
For ipsilateral lung, V10 and V5 were greatly reduced in DMLC (36.77 ± 2.31, 47.61 ± 2.84) but for tVMAT, V10 was more than the limits (43.95 ± 10.15) but V5 was well within the limit (56.94 ± 18.37). The V20, V30 and mean ipsilateral lung dose was less in DMLC.
Mean heart doses in DMLC and tVMAT were 2.61 ± 0.94 and 4.57 ± 2.61. Since we have taken right sided breast cases, dose received by 0.03 cc of heart was also noted which represents the maximum dose received by heart. D0.03 was much better in DMLC (24.72 ± 10.70) as compared to tVMAT (32.38 ± 9.65).
Mean contralateral breast dose was better in DMLC (2.39 ± 1.28) as compared to tVMAT (4.07 ± 1.70) although both the plans were well within the limits. Maximum dose to contralateral breast were almost similar.
All other OARs like contralateral lung, esophagus, spine, thyroid and liver were slightly better in DMLC as compared to tangential VMAT which can be concluded from (Table 1).
For integral dose evaluation, volume of 50% isodose line and 20% isodose line were noted. Volume of 50% isodose line (3409.63 cc) as well as 20% isodose line (4296.85) was greatly reduced in DMLC as compared to VMAT (3626.70 versus 4750.48 respectively).
Total number of monitor units required for delivering both the treatment plans was comparable.
DMLC plans (297.93 sec) required more time for delivery as compared to tVMAT (129.48 sec). DMLC plans require gantry rotation during the treatment, so that time was also included in treatment delivery time.
Similarly optimization time was more in DMLC. But, number of optimization required for one individual plan was more for tVMAT.
Conclusion
In summary, 6-beam DMLC treatment planning techniques are more suitable for treatment of BCS patients with a more convex breast or patients with barrel-shaped chest. The tVMAT plans are more conformal but their utility is limited with beam arc angles and also have increased lower-dose areas in organ at risks especially lungs. The evaluated DMLC plan in this study provided a very useful replica of tangential VMAT. With this DMLC technique, the dose distribution can be further optimized to obtain better sparing of various OARs with improved coverage of treatment volumes and less integral dose. Although, the tangential VMAT plan optimization is a less time-consuming technique than DMLC, majority of our DMLC plans using Monaco planning stations had good optimization in initial run only. In the end, this analysis is completely applicable on Left side convex chest wall patients as well.
References
- NIH consensus conference (1991) Treatment of early-stage breast cancer. JAMA 265: 391-395.
- Goldhirsch A, Glick JH, Gelber RD, Senn HJ (1998) Meeting highlights: International Consensus Panel on the Treatment of Primary Breast Cancer. J Natl Cancer Inst 90: 1601-1608
- Moody AM, Mayles WP, Bliss JM, A Hern RP, Owen JR, et al. (1994) The influence of breast size on late radiation effects and association with radiotherapy dose inhomogeneity. Radiother Oncol 33: 106-112.
- Early Breast Tribalism’s Collaborative Group (1995) Effect of radiotherapy and surgery in early breast cancer: An overview of the cancer trials. Nengl J med 333: 1444-14450.
- Clark BM, Wilkinson W, Ahoney LJ, Reid JG, Macdonald WD, et al. (1982) Breast cancer: A 21year experience with conservative surgery and radiation. Int J Radiate Oncol 8: 967-975.
- Hong L, Hunt M, Chui C, ForsterK, Lee H, et al. (1982) Intensity-modulated tangential beam irradiation of the intact breast. Int J Radiat Oncol Biol Phys 44: 1155-1164.
- Sailbishkumar EP, Mackenzie MA, Serine D, Mihai A, Hanson J, et al. (2008) Skin-sparing radiation using intensity-modulated radiotherapy after conservative surgery in early-stage breast cancer: A planning study. Int J Radiat Oncol Biol Phys 70: 485-491.
- Larry L, Michael B, Robert C, Vicini FA, Yan D, et al. (2000) Intensity modulation to improve dose uniformity with tangential breast radiotherapy: Initial clinical experience. Int J Radiat Oncol Biol Phys 48: 1559-1568.
- Donovan E, Bleakley N, Denholm E, Evans P, Gothard L, et a.l (2007) Randomised trial of standard 2D radiotherapy [RT] versus intensity modulated radiotherapy [IMRT] in patients prescribed breast radiotherapy. Radiother Oncol 82: 254-264.
- Jin GH, Chen LX, Deng XW, Liu XW, Huang Y, et al. (2013) A comparative dosimetric study for treating left-sided breast cancer for small breast size using five different radiotherapy techniques: Conventional tangential field, filed-in-filed, tangential-IMRT, multi-beam IMRT and VMAT. Radiat Oncol 8: 89.
- Jin GH, Chen L-X, Deng X-W, Liu XW, Huang Y, et al. (2013) A comparative dosimetric study for treating left-sided breast cancer for small breast size using five different radiotherapy techniques: Conventional tangential field, filed-in-filed, Tangential-IMRT, Multi-beam IMRT and VMAT. Radiat Oncol. 8: 89.
- Popescu CC, Olivotto IA, Beckham WA, Ansbacher W, Zavgorodni S, et al. (2010) Volumetric modulated arc therapy improves dosimetry and reduces treatment time compared to conventional intensity modulated radiotherapy for locoregional radiotherapy of left-sided breast cancer and internal mammary nodes. Int J Radiat Oncol Biol Phys 76: 287-295.
- Johansen S, Cozzi L, Olsen DR (2009) A planning comparison of dose patterns in organs at risk and predicted risk for radiation induced malignancy in the contralateral breast following radiation therapy of primary breast using conventional, IMRT and volumetric modulated arc treatment technique. Acta Oncol 48: 495-503.
- Coles CE, Moody AM, Wilson CB, Burnet NG (2005) Reduction of radiotherapy-induced late complications in early breast cancer: The role of intensity-modulated radiation therapy and partial breast irradiation. Part II-radiotherapy strategies to reduce radiation-induced late effects. Clin Oncol 17: 98-110.
- Mukesh MB, Harris E, Collette S, Coles CE, Bartelink H, Wilkinson J, et al. Normal tissue complication probability (NTCP) parameters for breast fibrosis: Pooled results from two randomised trials. Radiat Oncol 108: 293-298.
- Blom Goldman U, Wennberg B, Svane G, Bylund H, Lind P (2010) Reduction of radiation pneumonitis by V20-constraints in breast cancer. Radiat Oncol 5: 9.
- Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, et al. (2013) Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med 368: 987-998.
- A Munshi, B Sarkar, S Anbazhagan, UK Giri, H Kaur, et al. (2017) Short tangential arcs in VMAT based breast and chest wall radiotherapy lead to conformity of the breast dose with lesser cardiac and lung doses: A prospective study of breast conservation and mastectomy patients Australas Phys Eng Sci Med 40: 729-736.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences