Demographic Study of Changing (Core) Body Temperature in Categories of Human Subjects for Health Implication
Alao OA, Owolabi FM, Musiliyu KA
1Department of Physical and Mathematical Sciences, Afe Babalola University, Ado Ekiti, Ekiti State, Nigeria
2Department of Biomedical Technology, Federal University of Technology, Akure, Ondo State, Nigeria
- *Corresponding Author:
- Alao OA
Department of Physical and Mathematical Sciences, Afe Babalola University, Ado Ekiti, Ekiti State, Nigeria
E-mail: olumuyiwaalao@gmail.com
Received date: March 11, 2020; Accepted date: April 01, 2020 ; Published date: April 08, 2020
Citation: Alao OA, Owolabi FM, Musiliyu KA (2020) Demographic Study of Changing (Core) Body Temperature in Categories of Human Subjects for Health Implication. Insights Med Phys Vol.5 No.1:5. DOI: 10.36648/2574-285X.5.1.5
Copyright: © 2020 Alao OA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
The human demographic modelling is to show the levels of confidence between threshold temperature at the time of diagnosis and expected temperature to infer if there may be spontaneous metabolic heat production relative to atmospheric temperature indices. These were to show a pathway to grades of cold spells or heat waves in affected individuals and thermal sensitivity of the physiological temperature in human subjects. Climate change dynamics are observed through the study the weather variables which include; the surface and ambient temperatures, wind speed, relative humidity and dew points which may have positive or negative effects on human and environment. The impacts of changing climate have been found to affect human health through trails of varying complexity of these factors of the weather system. Human exposure to weather extremes; heat waves, cold spells and increases in other forms of extreme weather events give rise to ailments or disease factors such as heat stroke and influenza in individuals. Inclusively, the body unusual rising temperatures (hyperthermia) or body unusual low temperature (hypothermia) is an indication from infections with biotic factors (viral and bacterial), parasite and other air pollutant resulting from climate changes. This study have taken dare interest in observing the intense equilibrium between the factors of the weather systems and normal human body metabolism as to continue to maintain core(internal) temperature around (37 ± 1)°C for healthy human body.
Keywords
Climate change dynamics; Thermal sensitivity; Humidity controlled air temperature; Relative humidity; Physiological stress; Biotic factors
Introduction
Heat and cold related mortality is the result of excessive temperature related stress conditions experienced by the human body. The body’s heat regulatory function enables us to cope with exposure to high and low temperatures, but this coping increases the stress on many body functionalities especially regarding the cardiovascular circulation. Most studies therefore focus on ambient temperature, measuring a single or group of weather stations near cities or urban settlements as to quantify different conditions and level of heat stress. This are actually assumed to experience some error deviations due to the fact that the population under study is not systematically recorded. And also in cases where air conditionings are present, modifications are possible between the ambient temperatures and heat stress. However, the majority of studies focuses on daily average temperature, and also may involve the daily minimum and maximum temperatures in order to capture the differences in daytime and night-time exposures. In determining the heat index, some studies for control of relative humidity and dew temperature are calculated resulting in apparent temperatures which are based on the fact that the nonlinearities and threshold effect resulting in heat stress needed been accounted for. More creditable studies on the effect of temperature on mortality generally detect significant effects only on the lower and upper extremes of the distribution of temperature over the body. Nonetheless, empirical modelling of temperature for health implications are more accurately achieved through threshold indicators and other temperature instruments such as thermo-hygrometer used in this study. While these devises are used, discrete measures of daily temperature distributions are set in ranges and thus allow us to have a reference category in order to have a potentially differential impact on the health outcome.
Literature Review
Global climate changes have been found to affect human health through trails of varying complexity, scale and directness and with different timing. Also, impacts would vary geographically as a function both of environment and topography and of the vulnerability of the local population. The weather variables which include the temperature, wind speed, relative humidity and dew points have both positive and negative impacts although expert ’ s reviews anticipate predominantly negative. This condition is true since climatic change would interrupt or otherwise alter a large range of natural ecological and physical systems that are integral part of earth’s life- support system. Through climate change humans are contributing to a change in the conditions of life on Earth. The more direct impacts on health include those due to changes in exposure to weather extremes, heat waves, cold spells and increases in other extreme weather events with may include floods, storms, and droughts); and increased production of certain air pollutants. Understanding and interpretation of climate variables may compensate for possible increases from high frequency of heat waves and cold spell in a particular changing climate. The extent of change in the frequency, intensity and (location of extreme weather events due to climate change remains uncertain in an earth region or location. In the earth regions with a high level of excess cold, the beneficial impact may outweigh the detrimental, there are still time or periodic adaptation that are required [1,2]. Climate change, acting via less direct mechanisms, would affect the transmission of many infectious diseases especially water, food and vectorborne diseases and regional food productivity especially cereal grains. In the longer term and with considerable variation between populations as a function of geography and vulnerability, these indirect impacts are likely to have greater magnitude than the more direct [3,4]. For vector-borne infections, the distribution and abundance of vector organisms and intermediate hosts are affected by various physical factors; temperature, precipitation, humidity, surface water and wind and biotic factors; vegetation, host species, predators, competitors, parasites and human interventions [5]. However, the main pathways and categories of health impact of climate change are however shown in Table 1.
| Climatechanges | Modulatinginfluences | Healtheffects |
|---|---|---|
| Heatwaves | Transmission dynamics | Air pollution related health effect |
| Extreme weather | Agro-ecosystems | Extreme weather related health effects |
| Temperature | Socioeconomics, Demographics | Temperature related illness and death |
| Precipitations | Hydrology | Mental and nutritional infectious |
| Regional weather changes | Microbial contamination pathways | Water and food borne disease ,, |
Table 1: Showing the pathways by which climate change affects human health, including local modulating influences and the feedback influences of adaptation measures [5].
Methodology
This demographic study has taken a focus why human (patient) subjects are responsive to the changing (internal) body temperatures as a result of an infection commonly caused by exposure to biotic factors such as viral and bacterial. In this regard, the body unusual rising temperatures (hyperthermia) or body unusual low temperature (hypothermia) as an indication from infections with these biotic factors (viral and bacterial), parasite and other air pollutant resulting from changing climate has been threshold for many (if not all) ailments in individuals [6]. The equilibrium between the factors of the weather systems and normal human body metabolism needed be maintained for core (internal) temperature around (37 ± I) OC for a healthy human body. The comparison in this study shows the clinically recorded body temperature at the time of ailment and the expected temperature for health reasons. It is observed that the effect of surface (transient) temperature on human skin generally exposed to significant measures of the lower and upper extremes of the distribution of temperature over the body only contributes independently. Based on 2013/2014 procedure of the Centre for Disease Control and Protection (CDC), the expected core (internal) body temperatures indices for different human subjects are shown in Table 2. These are to provide information on physiological thermal human body sensitivity under comparative weather systems [7,8]. This is to observe the level of the effects of the components of the weather system which include the air temperature, air humidity and wind speed in order to know the causative factors influencing on the human energy balance during the exposure to extreme weather conditions [9]. However, the strong influence on thermo physiological significant indices of physiological temperature and its equivalents are depending on relevant indices for the human energy balance (Table 3).
| Human group | Age range | Reading type | Expected (core) body Temperature (/°C) |
|---|---|---|---|
| Infants | <2 years | Rectal | 36.6 |
| Child | 2 years | Rectal | 37.5 |
| Child | = 2 years <5 years | Rectal | 38 |
| Child | = 5 years =11 years | Rectal | 36.4 |
| Adolescence | = 12 years = 18 years | Oral | 37.6 |
| Adults | >18 years | Armpit | 35.2 |
| Aged | = 65 years | Oral | 38.1 |
Table 2: Demographic indices for changing body temperature in human subjects.
| Human subjects | Age | Type of reading | Clinical recorded temp. (/°C) | Core/Normal temp. expected (/°C) | Ailment type | Temperature difference |
|---|---|---|---|---|---|---|
| Infant (Child) | 3 months | Rectal | 38 | 36.6 | Fever | 1.4 |
| Child | 2 yrs | Rectal | 38 | 37.5 | Fever | 1.4 |
| Child | 2 yrs | Rectal | 38 | 37.5 | Rubeola | |
| Child | 3 yrs | Armpit | 37.2 | 35.2 | High blood pressure | 0.2 |
| Child | 3 yrs | Armpit | 37.2 | 35.2 | Dehydration (Diarrhea) | 0.2 |
| Child | 5 yrs | Rectal | 38.1 | 38 | Measles | 0.1 |
| Child | 5 yrs | Rectal | >38.0 | 38 | Roseola | |
| Child | 10 yrs | Oral | 38 | 37.5 | Malaria fever | 0.5 |
| Child | 11 yrs | Rectal | 38 | 36.4 | Roseola | 1.6 |
| Adolescence | 12 yrs | Oral | 38 | 37.6 | Malaria fever | 0.4 |
| Adolescence | 12 yrs | Armpit | 32.2 | 37.6 | Hypertension | 5.4 |
| Adult | Ad | Oral | 39.5 | 35.2 | Hyperpyrexia | 4.3 |
| Adult | Ad | Oral | 41 | 37.6 | Very high fever | 3.4 |
| Adult | Ad | Armpit | 37.6 | 36.9 | (Hypoglycemia/low blood sugar) | 0.7 |
| Adult | Ad | 28 | 36.9 | (Pulmonary edema) | 8.9 | |
| Adult | Ad | Oral | 37.5 | 38.1 | Cancer in blood | 0.6 |
| Adult | Ad | Oral | 38 | 38.1 | Migraine | 0.1 |
| Adult | Ad | Oral | 37.6 | >37.0 | Low blood sugar (Diabetes/hyperglycemia | >0.6 |
Table 3: Expected core (internal) body temperatures indices in categories of human subjects.
Results and Discussion
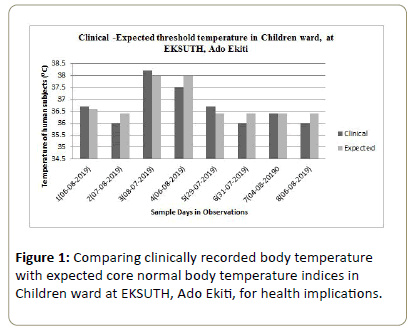
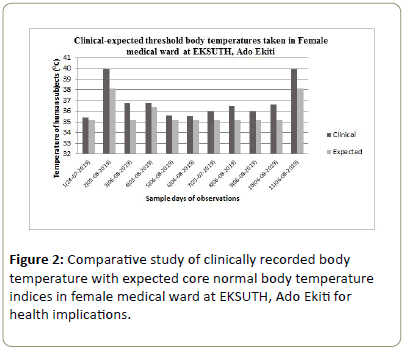
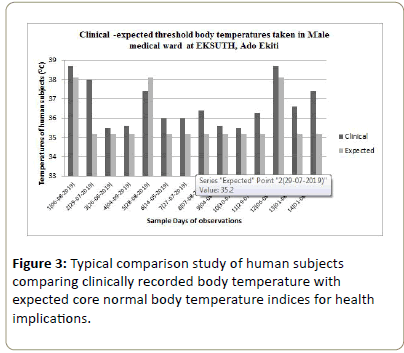
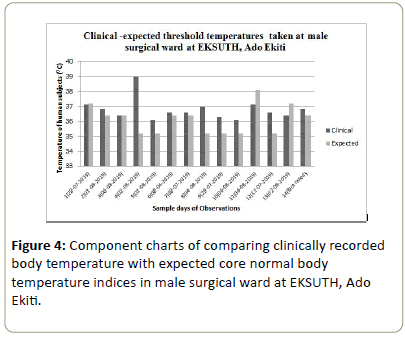
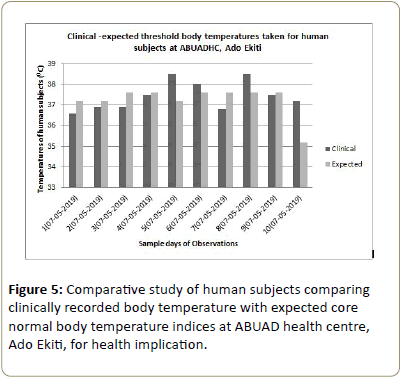
Comparative study of clinically – threshold body temperature in human subjects with expected core (healthy) body temperatureThe analysis of the hospital–healthcare data is from the report of secondary data that showed the latitude of the core–body threshold temperatures in Figures 1-5. The clinical/expected human subjects’ body temperature at the health care centers (Ekiti State Teaching Hospital (EKSUTH) and Afe Babalola health centers at Ado Ekiti) indicates the differences for the diagnosis made on individuals at the time of admission. The indication inferred is that not only biotic factors are responsible for the rise/fall in body temperature while admitted but also some spontaneous reactions such as anxiety, pain and fear contribute to increasing rise/fall in core-body temperature. The independent factors are responsible for extreme physiological stress resulting from thermal sensitivity of the environment causing heat or cold related diseases. Also air pollutants are factors of changing climate that induces temperature related stresses. This is obvious from the survey or diagnoses taking on surgery or emergency situation from the hospital recorded reports (Figure 4). The rationalization of clinical/ expected threshold temperatures are statistically discussed on confidence interval, thus 95% confidence limit for ratio more than unity and 99% confidence on unity level.
For other situation lower than the limits, the cases are considered abnormally unstable for temperature conditions. The relationships between core body temperature and the atmospheric temperature is the increase in temperature in air that cause biotic factors to increase index of ailment or diseases. The severity of the rise/fall in temperature is remarked stable, normal or abnormally unstable. The notes and inferences of the reports taking for level of stability calculated in ratio that determines the confidence advantages and possibility of normal/stable temperature body situations and abnormal unstable conditions.
Conclusion
The time series of the study of temperature have been in the interest of observing the intense equilibrium of the extreme weather conditions which are characterized by heat waves and cold spells. However, in order to maintain the internal temperature around 37°C for healthy human body only with variations usually of less than 1°C at a particular time of the day based on level of physical activity or emotional state, some factors of the weather system are taken into considerations. Nonetheless, the rising temperatures or extremely low temperatures may result in diseased climates. The increase in the temperature of atmosphere results in hot spots and contributes to availability in the surface properties of changes in the habitat that may have influence on animal and human health. This study has conversely observed the moisture advantages of our saturated cloud under intense temperature effects.
References
- Langford IH, Bentham G (1995) The potential effects of climate change on winter mortality in England and Wales. Int J Biometeorology 38: 141–147.
- Rooney C (1998) Excess mortality in England and Wales during the 1995 heat-wave. J Epidem Com Health 52: 482–486.
- McMichael AJ, Githeko A (2001) Human health in: Climate Change
- Epstein PR (1999) Climate and health. Science 285: 347–348.
- Patz J, McGeehin MA, Bernard SM, Ebi KL, Epstein PR, et al. (2000) The potential health impacts of climate variability and change for the United States. Environmental Health Perspectives 108: 367–376.
- Curwen M, Devis T (1988) Winter mortality, temperature and influenza: has the relationship changed in recent years? Population Trends 54: 17–20 .
- Drinkwater B, Horvath S (1979) Heat tolerance and ageing. Med Sci Sports and Exercise 11: 49–55.
- Mayer H (1993) Urban bioclimatology. Experientia 49: 957-963.
- Kilbourne EM (1992) Illness due to thermal extremes. In: Public health and preventative medicine, pp: 491–501.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences