Evaluation of Radiation Safety Parameters from Patients Receiving I-131 Therapy for Thyroid Carcinoma
Abdulrahman Mofreh Al-Esaei1, Emran Eisa Saleh2*, Sharief El Maghraby3, Tamer Mahmoud El Sayed4 and Amr Mohamed Ismail Kany5
1.Department of Physics, Al-Azhar University, Cairo, Egypt 2.Department of Physics, University of Aden, Aden, Yemen 3.Department of Oncology, Cairo University, Cairo, Egypt 4.Department of Physics, Al Azhar University, Cairo, Egypt 5.Department of Physics, Al Azhar University, Cairo, Egypt
Published Date: 2024-02-28DOI10.36648/2574-285x.9.1.50
Abdulrahman Mofreh Al-Esaei1, Emran Eisa Saleh2*, Sharief El Maghraby3, Tamer Mahmoud El Sayed1 and Amr Mohamed Ismail Kany1
1Department of Physics, Al-Azhar University, Cairo, Egypt
2Department of Physics, University of Aden, Aden, Yemen
3Department of Oncology, Cairo University, Cairo, Egypt
- *Corresponding Author:
- Emran Eisa Saleh
Department of Physics, University of Aden, Aden,
Yemen,
Tel: +201555049233,
E-mail: eesas2009@yahoo.com
Received date: February 18, 2024, Manuscript No. IPIMP-24-18668; Editor assigned date: February 20, 2023, PreQC No. IPIMP-24-18668 (PQ); Reviewed date: February 23, 2024, QC No. IPIMP-24-18668; Revised date: February 26, 2023, Manuscript No. IPIMP-24-18668 (R); Published date: February 28, 2024, DOI: 10.36648/2574-285x.9.1.52
Citation: Al-Esaei AM, Saleh EE, Maghraby SE, El Sayed TM, Kany AMI (2024) Evaluation of Radiation Safety Parameters from Patients Receiving I-131 Therapy for Thyroid Carcinoma. J Med Phys Appl Sci Vol.9 No.1:52.
Abstract
Background: Patients with thyroid cancer who receive I-131 treatment in radiotherapy centers are considered a source of external dose received by the workers in these centers as well as the family and the population.
Objective: To evaluate the External Dose Rate (EDR) and Retained Body Activity (RBA) as a function of time and distance during administration of I-131, as well as calculate the urinity radioiodine excretion.
Methods: One hundred and fifty patients were recruited and divided into two groups: The ablation Group (A) and the follow-up Group (B) the EDR, RBA and urinity radioiodine excretion were measured using a digital radiation dosimeter.
Results: Equations have been demonstrated to calculate the EDR and the RBA as a function of time (h) at distances of 0.1, 0.5, 1, 2 and 3 m after administration of I-13. Also urinary iodine excretion in 20 patients for each group was measured to find out the excretion of radioiodine into domestic drainage system.
Conclusion: The equations that were established to calculate the EDR as well as the RBA for a period of up to 96 hours after I-131 administration are useful for estimating radiation doses from patients at radiotherapy centers and could help the workers to minimal exposure.
Radiotherapy; I-131; External dose rate; Patients; Retained body activity
Introduction
The increasing use of radionuclides in the diagnosis and treatment of incurable diseases such as thyroid carcinoma and the exposure to ionizing radiation, whether for workers in the field of radiation therapy or the nursing staff, requires great efforts in assessing the radiation doses resulting from the use of these radionuclides [1-2].
Recently, the use of radionuclides has increased in the diagnosis and treatment of malignant diseases in nuclear medicine and radiotherapy centers, including the radioactive iodine isotope (I-131) used in the treatment of thyroid cancer [3-4]. The potential radioactive risk in radiotherapy centers results from the use of radioactive iodine isotope I-131 in the treatment of thyroid carcinoma. These risks include emitted gamma rays, as well as the release of radioactive isotopes in urine, perspiration, saliva and breath. Patients treated with radioactive iodine is considered a source of radioactive contamination, which can be a cause of external radiation exposure due to the high energy, penetrating power and ionization of gamma rays [5].
The International Commission on Radiation Protection (ICRP) and the International Atomic Energy Agency (IAEA) have set their recommendations for the annual dose that any member of the public should be allowed to receive within the limits of less than 5 mSv y-1 [6,7]. The radiation dose received by the workers in the radiotherapy centers from the patient depends on several factors, the most important of which are: The distribution of iodine inside the patient’s body, the rate of iodine clearance and the time that the person spends in close proximity to the patient [8]. According to the IAEA, the rate of radiation dose must be less than 70 μSv h-1 at a distance of 1 m from the patients to release them. Also, European Union (EU) regulations stipulate that the external dose rate for patients receiving I-131 must be reduced to less than 20 μSv h-1 at 1 m to release them [9].
Several researches have focused on the evaluation of external dose rate resulting from I-131 at radiation therapy centers. Barrington et al. [10] measurements the whole-body dose rate for 86 thyroid cancer patients and calculate the accumulative dose to staff resulting from the contact with the patients and also calculate the urinary iodide excretion in 19 patients. The estimated of accumulative doses to nursing staff were found to be from 0.08 to 6.3 mSv for ablation group and were 0.18 to 12.3 mSv for the follow-up group. Zhang et al. [8] study external dose rate and retained body activity of 70 patients. The results show the external dose rate were 19.2, 8.85, 5.08 and 2.32 μSv h-1 at 1, 1.5, 2 and 3 m and the retained body activity was <400 MBq. Klain et al. [3] measure the whole-body radioiodine effective half-life in 166 patients. The results show the whole body radioiodine effective half-life ranged from 4.08 h to 56.4 h.
The aims of current work to evaluate the external dose rate received by staff in radiotherapy centers and measure retained body activity in the patients resulting from the receiving I-131 I for treatment thyroid carcinoma.
Materials and Methods
Patients materials
The study was carried out in two different radiation therapy center in Cairo, Egypt. This study was approved by our academic and medical institution review board. Written consent was obtained from all patients after clarifying the objectives of the study and explaining the method. One hundred and fifty patients were recruited. The patients were divided into two groups: The ablation Group (A) which includes 75 patients and this group receiving I-131 for the first time after surgery and the follow-up; Group (B) which includes 75 patients receiving I-131 treatment for the second time. All patients' data including age, sex, etc. were recorded and the average was plotted in Tables 1 and 2. All patients had previously been treated with complete or near-total thyroidectomy. The administered activity for Group (A) was 2682.5 ± 1018 MBq (1850-3700 MBq) and for follow up; Group (B) was 4810 ± 829 MBq (3700-5550 MBq).
| Age (y) | Sex Female/Male | No of cases (n) | Average administrated activity (GBq) | Average dose rate at 1 m (μSv/h/MBq) | Average body shielding factor |
|---|---|---|---|---|---|
| ≤ 38 | F | 5 | 2.3 ± 0.4 | 0.031 ± 0.005 | 0.51 ± 0.08 |
| M | 3 | 2.5 ± 0.6 | 0.028 ± 0.002 | 0.46 ± 0.03 | |
| 39-50 | F | 21 | 2.4 ± 0.3 | 0.031 ± 0.003 | 0.51 ± 0.05 |
| M | 10 | 2.6 ± 0.7 | 0.029 ± 0.001 | 0.48 ± 0.02 | |
| 51-60 | F | 11 | 2.8 ± 0.9 | 0.025 ± 0.003 | 0.41 ± 0.05 |
| M | 6 | 2.9 ± 0.6 | 0.024 ± 0.003 | 0.40 ± 0.05 | |
| 61-70 | F | 5 | 2.7 ± 0.8 | 0.027 ± 0.002 | 0.45 ± 0.03 |
| M | 10 | 3.1 ± 0.6 | 0.023 ± 0.003 | 0.38 ± 0.05 | |
| ≥ 70 | F | 1 | 3 | 0.024 | 0.4 |
| M | 3 | 3.2 ± 0.4 | 0.023 ± 0.002 | 0.38 ± 0.03 | |
| All age | F | 43 | 2.4 ± 0.6 | 0.027 ± 0.003 | 0.45 ± 0.05 |
| M | 32 | 2.8 ± 0.5 | 0.025 ± 0.002 | 0.42 ± 0.04 | |
| All cases | 75 | 2.7 ± 0.6 | 0.026 ± 0.003 | 0.44 ± 0.05 |
Table 1: Patient parameters, administrated activity and average dose rate at 1 m for ablated Group (A).
| Age (y) | Sex Female/Male | No of cases (n) | Average administered activity (GBq) | Average dose rate at 1 m (μSv/h/MBq) | Average body shielding factor |
|---|---|---|---|---|---|
| ≤ 36 | F | 6 | 4.1 ± 0.4 | 0.020 ± 0.002 | 0.33 ± 0.03 |
| M | 1 | 3.7 | 0.022 | 0.36 | |
| 37-40 | F | 7 | 4.3 ± 0.6 | 0.020 ± 0.008 | 0.33 ± 0.13 |
| M | 5 | 4.2 ± 0.5 | 0.020 ± 0.006 | 0.33 ± 0.1 | |
| 41-50 | F | 15 | 4.7 ± 0.9 | 0.019 ± 0.008 | 0.31 ± 0.13 |
| M | 13 | 4.6 ± 0.8 | 0.019 ± 0.008 | 0.31 ± 0.13 | |
| 51-60 | F | 12 | 4.8 ± 0.7 | 0.019 ± 0.002 | 0.31 ± 0.03 |
| M | 11 | 5.3 ± 0.2 | 0.018 ± 0.005 | 0.30 ± 0.08 | |
| ≥ 60 | F | 1 | 5.6 | 0.017 | 0.28 |
| M | 4 | 5.2 ± 0.3 | 0.018 ± 0.006 | 0.3 ± 0.1 | |
| All age | F | 41 | 4.7 ± 0.6 | 0.019 ± 0.007 | 0.31 ± 0.08 |
| M | 34 | 4.6 ± 0.4 | 0.019 ± 0.006 | 0.32 ± 0.10 | |
| All cases | 75 | 4.7 ± 0.5 | 0.019 ± 0.007 | 0.32 ± 0.09 |
Table 2: Patient parameters, administrated activity and average dose rate at 1 m for follow up Group (B).
Measurement EDR and RBA
The external dose rate was measured for the patient’s administrated I-131 using a digital radiation dosimeter model ranger radiation alert. The range of the digital dosimeter is from 0.01 μSv.h-1 to 1 mSv.h-1. Digital dosimeter was calibrated annually at the Egyptian National Atomic Energy Authority. Dose rates for all patients were measured at the mid-frontal trunk at different distances of 0.1, 0.5, 1, 2 and 3 meters at time 2, 12, 24, 36, 48, 60, 72, 84 and 96 hours after administration of I-131. The external dose rate was measured from the patients in a private room and the radiation background was taken into account and it was subtracted from the average radiation dose obtained from the patient. Three measurements were taken at each time and the average was taken for each measurement.
For the purpose of measuring Retained Body Activity (RBA), urine collections were obtained for 20 patients from each group for up to 5 days after the administration of I-131 to measure urinary iodide excretion. Urine was collected immediately after administration of I-131 and collected in graduated containers for 24 hours. The container was stirred to ensure even distribution of radionuclides through the urine and was counted in a standard isotope (CRC-55tR, Ramsey, NJ 07446, USA). A 5 ml of urine from each sample was taken to measurement the activity of urine. After each measurement, the urine was discarded and new containers were used. The retained I-131 body activity was estimated by using the following equation:
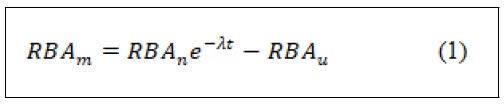
Where RBAm is RBA at m h, RBAn is RBA at n h (m>n) and RBAu is the activity in the urine between m and n h.
Results and Discussion
The selected of the radioactive isotope I-131 of iodine in the treatment of the thyroid carcinoma is due to the ability of the thyroid cells to absorb it. Emission of beta particles from this isotope destroys cancerous cells in the thyroid gland. In addition to the emission of beta particles from this isotope, it also emits gamma rays with different energies, which leads to the possibility of radiation hazards for workers at radiotherapy centers and patient companions due to the ability of gamma rays to high permeability and ionization [5].
External Dose Rate (EDR)
This study was carried out on 150 patients who were diagnosed with thyroid cancer and the patients were divided into two groups, Ablation Group (A) and follow up Group (B), each group consisted of 75 patients. For ablation Group (A) 57% were females and 43% were males. The majority of these patients (about 84%) were in the age group from 38 to 70 y, 5.3% were above 70 y and 10.6% were less 38 y. For follow up Group (B) 54.6% were females and 45.3% were males. The majority of these patients (about 84%) were in the age group 36-60 y, 9.3% were less 36 y and 5.7% were above 60 y.
In terms of activity administration, the values ranged between 1.85 to 3.70 GBq for Group (A) with the average value of 2.7 ± 0.6 GBq and between 3.70 to 5.55 GBq with the average value of 4.7 ± 0.5 GBq for Group (B).
Table 1 shows age, sex, administration activity and radiation dose rate at a distance of 1 meter, as well as the body shielding factor for Group (A). Table 2 Shows the same date for Group (B). From the tables the averages radiation dose rate for Group (A) were about 0.027 ± 0.003 and 0.025 ± 0.002 μSv h-1/MBq for females and males respectively. The corresponding values for follow up Group (B) were 0.019 ± 0.007 and 0.019 ± 0.006 for females and males respectively. The results show the females had a higher EDR compared to the males for all groups. Also, the External Dose Rate (EDR) was measured at a distance of 0.1, 0.5, 1, 2 and 3 m from the patients who received I-131.
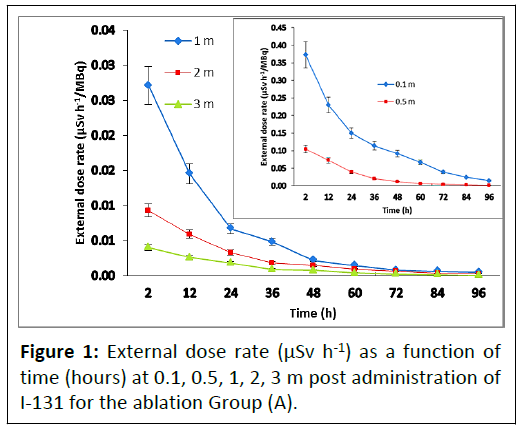
The value of the EDR at 2 hours after I-131 administration was chosen to be 100%. To facilitate the comparison process, the EDR was normalized with the administration activity. The mean external dose rate EDR was set in a monoexponential curve for the ablation Group (A) according to the following equations are shown in Figure 1.
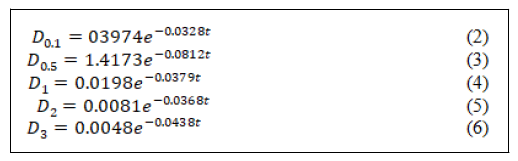
Where D0.1, D0.5, D1, D2 and D3 are the external dose rate at 0.1, 0.5, 1, 2 and 3 m distances, respectively and t is the time after the initial dose rate.
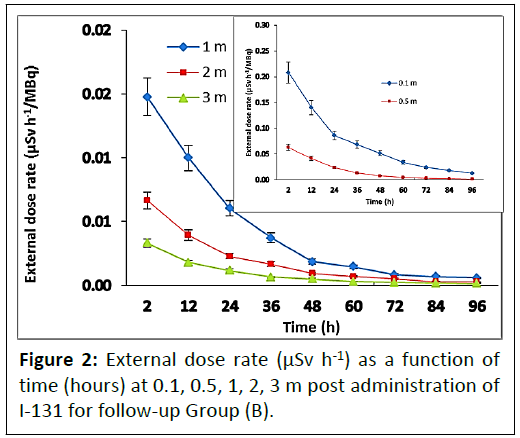
The mean EDR for follow up group decreased according the monoexponintially equations are shown in Figure 2.
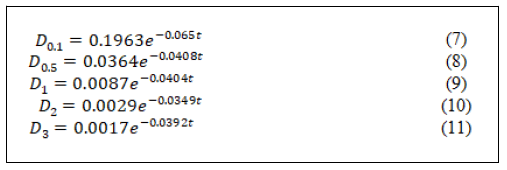
According to the previous equations, the EDR for the ablation Group (A) at time 2, 12, 24, 36, 48, 60, 72 and 96 and at 1 m distance were: 0.0271 ± 0.0040, 0.0145 ± 0.0022, 0.0067 ± 0.0015, 0.0048 ± 0.0012, 0.0022 ± 0.0010, 0.0015 ± 0.0005, 0.0008 ± 0.0003, 0.0006 ± 0.0002 and 0.0005 ± 0.0002 μSv h-1 MBq-1 respectively. The corresponding value for follow up group were 0.0100 ± 0.0025, 0.0054 ± 0.0015, 0.0025 ± 0.0012, 0.0018 ± 0.0005, 0.0008 ± 0.0003, 0.0006 ± 0.0003, 0.0003 ± 0.0002, 0.0002 ± 0.0001 and 0.0002 ± 0.0001 μSv h-1 MBq-1 respectively.
It can be seen from the results, the mean dose rates for ablation Group (A) at 1 m distance were higher than the corresponding value for follow up Group (B). This result is agreed with that obtained by the Barrington et al. and Zhang et al. [8,10]. Also as can be seen from the results that the EDRs from follow up Group (B) decreased faster than the EDRs from ablation Group (A). The median and the upper 95th percentile values for patients under study were (0.026 and 0.033) and (0.019 and 0.023) μSv h-1 MBq-1 for Group A and Group B respectively. The upper 95th percentile values of this study were lower than the corresponding values reported by Barrington et al. and Al-Hag et al. [5,10] in British and Saudi Arabia thyroid cancer (0.066 and 0.042 μSv h-1 MBq-1) respectively.
Retained Body Activity (RBA)
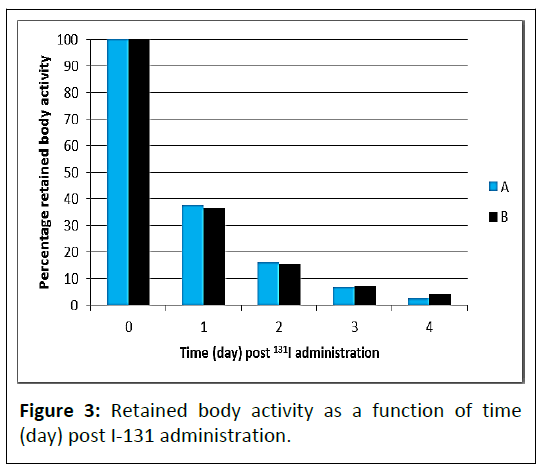
After a patient of thyroid cancer administration I-131, the body gets rid of it by many methods and the urinary system is the main pathway for that, although there are other ways such as sweat, saliva and exhalation [11]. Retained body activity was calculated by calculating the activity present in the urine and subtracting it from the administered activity of I-131 after correcting for time attenuation. The results are presented in Figure 3. From the Figure, it is clear that even though the administration activity of the group (A) was higher than Group (B), the group (B) cleared the I-131 activity faster than Group A. The reason for that due to the Group (B) had almost completely ablated the thyroid tissue, so that the absorption of I-131 was less than the ablated Group (A), which was retained in the thyroid tissue or part of it.
The activity of I-131 in the two group was decreased monoexponentially as the following equation:
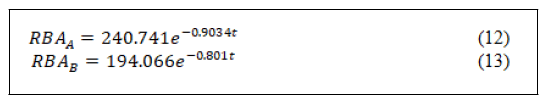
According to the equations 12 and 13 and as shown in Figure 3, it is clear that the RBA decreased rapidly during the first 24 hours and after 96 hours the RBA becomes low enough that it does not pose a significant risk to the population [12]. Therefore, it is recommended the release time when the administration activity becomes less than 400 MBq or <20 μSv h-1 [13]. The release time for patients for Group (A) and (B) were 21 and 23 h.
Effective half-life (Teff) and body Shielding Factor (SF)
The effective half-life (Teff) was calculated for all patients using the values of the serial external dose rate [5]. The mean value of the effective half-life Teff for both groups was about 18.3 ± 8.1 and 17.1 ± 7.3 h for the ablation Group (A) and follow up Group (B) respectively.
The highest value of the Teff was about 21 h and the lowest value was about 8.5 h. This result is consistent with the previous study by Damir et al. [14] where they found that the average Teff for patients was 18.7 ± 1.9 h, while it was less than the results found by Al-Hajj et al. [5] for 311 patients in Saudi Arabia (12-14 h), as well as North et al. [15] and Willegaignon et al. [16], where the average Teff was about 14 and 11.41 h respectively. Also, the result of our study was lower than Kramer et al. [17] where they found the average Teff was about 21 h.
The mean body Shielding Factor (SF) was found for all patients by measuring the external dose rate at 1 meter distance and 2 hours after receiving the administered activity and the decay rate constant T=0.06 μSv MBq-1 h-1 for I-131 [5,18]. The mean and range value of the body shielding factor SF for Group (A) were 0.44 (0.38-0.51) and for Group (B) were about 0.32 (0.28-0.36). Females patients from Group (A) had SF (0.45) higher than males (0.42), conversely, males had SF (0.31) slightly higher than females patients (0.32) for Group B. The average SF in this work is lower than obtained (0.46) by Al-Haj et al. [5] and (0.6) by Siegel et al. [18].
Urinary I-131 excretion
The average daily percentage of activity for I-131 excreted in the urine for 20 patients of the ablated Group (A) and the 20 patients for the follow up Group (B) are shown in Table 3. The percentages of I-131 excreted during 24 and 48 h for ablated Group (A) were 64.31 and 83.48% and for follow up group were 65.60% and 83.79%. From the results it can be noticed the largest proportion of the activity is excreted within 48 hours after the activity administration. In comparison with other studies Willegaignon et al. [16] found that the percentages of excreted activity in the urine during the 24 and 48 h were 72%and 91%, respectively. Driver et al. [19] also found that the percentages of activity excreted in urine during the same time were 55% and 85%. Damir et al. [14] also found the percentages of activity excreted in urine at 24 and 48 h were about 66 and 87% which slightly higher than the present work.
| Days | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Mean Group (A) | 44.17 ± 8.8 | 13.17 ± 2.6 | 9.01 ± 1.80 | 1.66 ± 0.50 | 0.67 ± 0.013 |
| Mean Group (FU) | 55.51 ± 11.10 | 15.33 ± 3.06 | 10.84 ± 2.17 | 2.00 ± 0.04 | 0.86 ± 0.02 |
Table 3: Percentage of administrated activity excreted in urine.
Conclusion
Through this work, equations were established to find the EDR during the times up to five days and at distances of 0.1, 0.5, 1, 2 and 3 m. Also, equations were demonstrated to calculate the RBA by measuring EDR for patients receiving I-131 therapy. This work allows the creation of a database system through experiments to provide outlines of radiation exposure in radiotherapy centers. According to the regulations, the rate of external dose rate to release patients should be less than 20 μSv h-1, so the results of this work showed that the activity in the urine was rapid during the 24 hours following the administration activity and that the time required to discharge the patients was 21 and 23 hours after the administration activity for Group A and Group B respectively. Also this procedure differs from one patient to another according to the value of the administration activity.
Funding
No funding.
Competing Interests
The authors declare no conflict of interest, financial or otherwise.
Ethics Approval and Consent to Participate
Not applicable.
References
- Al-Esaei A, Khalil MM, El Shazly RM, Kany AMI, Saleh EE, et al. (2022) Assessment of radiation exposure dose for nuclear medicine workers from 18F-FDG, 99mTc MDP, and 99mTc. Curr Radiopharm15: 320-326.
[Crossref], [Google Scholar], [Indexed]
- Fathy M, Khalil MM, Elshemey WM, Mohamed HS (2019) Occupational radiation dose to nuclear medicine staff due to TC99m, F18-FDG PET and therapeutic I-131 based examinations. Radiat Prot Dosim 186: 443-451.
[Crossref], [Google Scholar], [Indexed]
- Klain M, Nappi C, Risi MD, Piscopo L, Volpe F, et al. (2021) Whole-body radioiodine effective half-life in patients with differentiated thyroid cancer. Diagnostics 11: 1740.
[Crossref], [Google Scholar], [Indexed]
- Deandreis D, Rubino C, Tala H, Leboulleux S, Terroir M, et al. (2017) Comparison of empiric versus whole-body/-blood clearance dosimetry-based approach to radioactive iodine treatment in patients with metastases from differentiated thyroid cancer. J Nucl Med 58: 717-722.
[Crossref], [Google Scholar], [Indexed]
- Al-Haj AN, Lagarde CS, Lobriguito AM (2007) Patient parameters and other radiation safety issues in I-131 therapy for thyroid cancer treatment. Health Phys 93: 656-666.
[Crossref], [Google Scholar], [Indexed]
- International Commissioin on Radiological Protection (ICRP) (2004) Release of patients after therapy with unsealed radionuclides. Ann ICRP 34: 5-6.
- (2006) Nuclear medicine resources manual. International Atomic Energy Agency, Vienna, Austria.
- Zhang H, Jiao L, Cui S, Wang L, Tan J, et al. (2014) The study of external dose rate and retained body activity of patients receiving I-131 therapy for differentiated thyroid carcinoma. Int J Environ Res Public Health 11: 10991-1003.
[Crossref], [Google Scholar], [Indexed]
- European Commission. Radiation Protection 97 (1998) Radiation Protection Following Iodine-131 Therapy (Exposures due to Out-Patients or Discharged In-Patient
- Barrington SF, Kettle AG, O’Doherty MJ, Wells CP, Somer EJR, et al. (1996) Radiation dose rates from patients receiving iodine-131 therapy for carcinoma of the thyroid. Eur J Nucl Med 23: 123-130.
[Crossref], [Google Scholar], [Indexed]
- Perrier ND, Brierley JD, Tuttle RM (2018) Differentiated and anaplastic thyroid carcinoma: Major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin 68: 55-63. [CrossRef] [PubMed].
[Crossref], [Google Scholar], [Indexed]
- Kumar P, Bal C, Damle NA, Ballal S, Dwivedi SN (2019) Lesion-wise comparison of pre-therapy and post-therapy effective half-life of Iodine-131 in pediatric and young adult patients with differentiated thyroid cancer undergoing radioiodine Therapy. Nucl Med Mol Imaging 53: 199-207.
[Crossref], [Google Scholar], [Indexed]
- Andres C, Barquero R, Tortosa R, Nunez C, Castillo AD, et al. (2011) I-131 activity in urine to the sewer system due to thyroidal treatments. Health Phys 101: 110-115.
[Crossref], [Google Scholar], [Indexed]
- Demir M, Parlak Y, Cavdar I, Yeyin N, Tanyildizi H, et al. (2013) The evaluation of urine activity and external dose rate from patients receiving radioiodine therapy for thyroid cancer. Radiat Prot Dosim 156: 25-29.
[Crossref], [Google Scholar], [Indexed]
- North DL, Shearer DR, Hennessey JV, Denovan GL (2001) Effective half-life of I-131 thyroid cancer patients. Health Phys 81: 325–329.
[Crossref], [Google Scholar], [Indexed]
- Willegaignon J, Stabin MG, Guimaraes MIC, Malvestiti LF, Sapienza MT, et al. (2006) Evaluation of the potential absorbed doses from patients based on whole-body I-131 clearance in thyroid cancer therapy. Health Phys 91: 123–127.
[Crossref], [Google Scholar], [Indexed]
- Kramer GH, Hauck BM, Chamberlain MJ (2002) Biological half-life of iodine in adults with intact thyroid function and in athyreotic persons. Radiat Prot Dosim 102: 129–135.
[Crossref], [Google Scholar], [Indexed]
- Siegel JA, Kroll S, Regan D, Kaminski MS, Wahl RL (2002) A practical methodology for patient release after Tositumobab and I-131 -Tositumomab therapy. J Nucl Med, 43: 354 –362.
[Google Scholar], [Indexed]
- Driver I, Packer S (2001) Radioactive waste discharge quantities for patients undergoing radioactive iodine therapy for thyroid carcinoma. Nucl Med Commun 22: 1129–1132
[Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences