Investigating the Effect of Ionizing Radiation on Intraocular Lenses at Clinical Doses
Spyratou E, John A, Kalliopi P, Constantinos B, MersiniMakropoulou, Alexander S and Efstathios Efstathopoulos
Spyratou E1, John A1, Kalliopi P1, Constantinos B2, MersiniMakropoulou2, Alexander S2 and Efstathios Efstathopoulos1*
1Department of Radiology, Medical School, National and Kapodistrian University of Athens, 11517 Athens, Greece
2Department of Physics, Faculty of Applied Mathematical and Physical Sciences, National Technical University of Athens, Zografou Campus, 15780 Athens, Greece
- *Corresponding Author:
- Efstathios Efstathopoulos
Department of Radiology, Medical School
National and Kapodistrian University of Athens
11517 Athens, Greece
Tel: +30 210 5831818
E-mail: stathise@med.uoa.gr
Received Date: June 04, 2017 Accepted Date: June 20, 2017 Published Date: June 24, 2017
Citation: Spyratou E, John A, Kalliopi P, et al. (2017) Investigating the Effect of Ionizing Radiation on Intraocular Lenses at Clinical Doses. Insights Med Phys. Vol. 2 No. 2: 6.
Abstract
Background: The natural crystalline lens of the eye is considered as one of the most radiosensitive tissues of the human body and long-time research demonstrates an association between ionizing radiation exposure and cataract development. Intraocular lens (IOL) implants are synthetic lenses used to replace the cataractous human lens of the eye and obtain optical rehabilitation in cataract surgery. However, post-operative complications such as capsular opacification, considerable cloudiness or discoloration may appear 2-3 years after the surgery. As the factors affecting the postoperative "life" of the IOL have not yet been fully clarified, in this study we examine if the irradiation with x-rays at clinical doses in interventional radiology and cardiology procedures of human eye can affect the transparency and clarity of the IOLs.
Methods and findings: A number of intraocular lenses with different polymer composition and refractive power (diopters) were studied. In this work we present the results obtained with 3yellow azo-dye doped IOL (Alcon) and 1 undoped hydrophobic acrylic IOL (Alcon) having the same diopter, that were irradiated toclinical doses of 25, 67, 600 (for the doped) and 300 mGy (for the undoped IOL) respectively. The transmittance of the IOLs was measured pre-irradiation and post-irradiation by using a spectralon-coated integration sphere and a UV/Visible spectrometer over the visible-near infrared spectrum range from 420-900 nm. The transmission spectra of the IOL pre and post-irradiation indicate that in the blue-green spectrum region from 420-550 nm theIOLs show an increase in the transmittance T, with a highest ΔΤ changeequal to 35%, 37%, 38% at 420 nm for doses of 25 mGy, 67 mGy and 600 mGy respectively. In the residual spectrum region from 550-900 nm the transmittance is decreased by percentage 2%, 5% and 6%, respectively. However, the transmission spectrum of the undoped IOL presents the same behavior in the blue-green region and a change in the transmittance at percentage 4% is observed in the spectrum region 550-900 nm after x-ray irradiation to dose of 300 mGy.
Conclusion: The results indicate that the irradiation with x-rays decreases the protection of the filter of the yellow azo-dye doped IOLs against the harmful for the retina UV radiation and short wavelength blue right, while affects slightly the transmittance in the residual visible-near infrared spectrum.
Keywords
Ionizing radiation; Blue-green spectrum; Cataractogenesis; Cholangiopancreatography; Transmittance
Introduction
The human visual system is complex, consisting of the cornea, the lens, and the retina. Over time, the normally crystal-clear lens can form cataract, which means that gradually loses its clarity, obstructing the passage of light for focusing on the retina. Hence, cataract is clouding the natural lens of the eye diminishing vision clarity up to the point of total blindness. It is now recognized that the cataract is a result of protein denaturation of the human lens due mainly to aging, while other causes may be metabolic changes, injury, radiation, toxic chemicals or drugs [1]. In parallel to the epidemiological findings, extensive work have been done to assess the exact mechanisms of radiation cataractogenesis and the evaluation of the minimal dose needed to cause cataract in the human eye, leading the International Commission on Radiological Protection (ICRP) initially to recommend threshold dose limits for visual-impairing cataracts of less than 2.0 Gy for low-LET ionizing radiation and less than 5.0Gy of protracted radiation [2]. Later, in Publication 118 (ICRP, 2012) [3], ICRP revised downwards its eye dose threshold for cataract induction to a current value of no more than 0.5 Gy, compared with the previous threshold doses for visual-impairing cataracts, further specifying a reduction in the dose limit for occupational exposure in planned exposure situations (in terms of equivalent dose) for the lens of the eye from 150 to 20 mSv per year [4,5]. Recently, Efstathopoulos et al. [6] investigating the occupational doses in 25 diagnostic and therapeutic interventional radiology and interventional cardiology procedures concluded that the interventionists receive 64-1129 μSv per procedure to the lens of the eye and the nurses 4-16 μSv. However, more epidemiological studies, especially at low radiation doses, are needed in order to have a more clear answer whether radiation-associated cataract is a deterministic or a non-threshold based effect [7].
Like cornea, the natural lens is nonvascular to ensure perfect light transparency. In addition, the lens has no loss of cells during its lifetime and no way of damaged cell repair or removal. Therefore, theonly effective treatment for cataract is the cataractous lens extraction and its replacement by an intraocular lens. The intraocular lenses made by traditional polymeric materials such as PMMA, which is suitably stained with substances e.g. yellowazo dyes that block the UV and blue-light radiation, but also by more modern flexible materials such as silicone and hydrophilic or hydrophobic acrylates [8-10]. However, many pathological processes lead to considerable cloudiness or discoloration of intraocular lenses, which are made of various biomaterials and different techniques [11]. Apart from factors related to patients’ associated conditions, the possible causes that affect the clarity of the IOL are the material and the manufacturing techniques, the storage process, the implantation technique, the degree of hydration and the exposure to the radiation [11,12].
The implantation of intraocular lenses increased extremely in our days, with a tendency to enter also in other ophthalmology disorders [13]. Thus, the monitoring of eye exposures to patients, physicians, and radiation workers which have IOL implants has become of increased interest. Despite the fact that several epidemiological studies were reported on cataract frequency in relation to radiation dose among persons exposed to ionizing radiation [14], only few experimental/clinical studies wereundertaken to investigate the effect of ionizing radiation on the optical properties of the implanted IOLs. In the relevant literature only one work has been published to determine whether x-ray radiation at clinical doses of human eye affects the UV-absorbing capacity of IOLs, resulting either to the retina exposure to potentially chronic UV damage, or to IOL transparency alteration [15]. In this work, authors conclude that at clinically relevant doses used in radiation therapy, megavoltage photon ionizing radiation to doses of 2, 5, 10, 20, 40, 60, and 100 Gray, produces no significant alterations in the absorption spectra of PMMA and silicone IOLs over the range of wavelengths in the range of 280– 830 nm [15]. An earlier study has reported to any possible disturbance of the dosimetric properties of the incident radiotherapy beam due to the presence of intraocular lenses within the path of a therapeutic radiation beam [16]. This research team embedded PMMA IOLs in polystyrene phantoms and observed a few percent attenuation of 6 MV photons beam, while they measured significant distortion in the radiation dosimetry of low-energy electrons beam of 6 MeV, with only 60% transmission, which is not a suitable choice to treat tumors behind ocular implants [16].
In our study we investigate the effect of the ionizing radiation on the optical properties of modern yellow azo-dye acrylic IOL (Alcon SN60WF model) after exposure to eye lens doses for patient and also for occupationally exposed medical staff which can receive during interventional radiology and cardiology procedures. According to the published data collected from European hospitals, occupational medical staff expose to a highest average dose of about 60 μSv per procedure in embolizations, while for endoscopic retrograde cholangio-pancreatography procedures (ERCP) a maximum eye lens dose of 4 mSv was measured, and for embolizations 2.5 mSv [17]. In literature, average doses in patient’s eyes of 380 mGy, with maximum of 2079 mGy have been reported during cerebral embolizations [18]. In another study on interventional neuroradiology doses, mean patient eyes doses of 67 mGy and 300 mGy have been recorded for diagnostic and therapeutic procedures respectively, while 16% of the therapeutic procedures measured higher that the threshold of 500 mGy to produce eye lens opacities according to the ICRP [19]. In this study we focus onany alterations on transparency in the visible spectrum range and on the UV-blue light protection filter of the IOLs after irradiation to doses of 25 mGy, 67 mGy, 300 mGy and 600 mGy.
Materials and methods
Materials and irradiation protocol
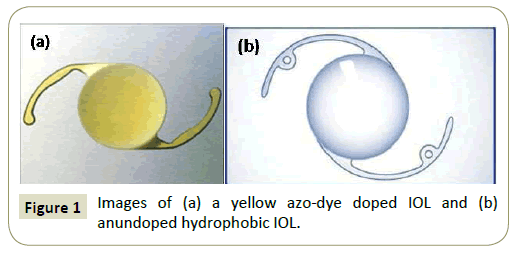
Two yellow azo-dye doped IOLs (SN60WF, SN60AT Alcon) were irradiated with x-rays at clinical doses of 25 and 67 mGy respectively while 1 yellow azo-dye IOL (SN6AD1, Alcon) was selected to be irradiated at 600 mGy, over the threshold of 500 mGy for the visual-impairing cataracts of eyelens (Figure 1). The yellow azo-dye IOLs are made from an acrylate/methacrylate Copolymer doped with a yellow azo dye providing a barrier against UV radiation and blue light region. In comparison, 1 undoped hydrophobic acrylic IOL (MA60BM Alcon) made from acrylate/ methacrylate copolymer with a bonded UVabsorber was irradiated at 300 mGy. The transmission spectra of the IOLs were recorded pre-irradiation and post-irradiation by using a spectralon-coated integration sphere and a UV/Visible spectrometer over the visible-near infrared spectrum.
Integrating sphere measurements
A Lab sphere integrating sphere (819C-SF-6, NRC Newport Research) with spectraflect coating and 6 port of 1 inch in diameter each was connected with a USB 4000 UV/Vis spectrophotometer (Ocean Optics) operating in the wavelength range from 360-1100 nm. The light source was a LS-1Tungsten lamp (ocean optics) operating in 360-2400 nm. According to Akinay et al. [20], the use of an integrating sphere for light transmission measurements of intraocular lenses demonstrated the appropriateness for that in both industry and academia, compared to generally used double-beam spectrophotometers. The IOL under analysis was placed into a plastic custom insert that had a 5-mm-diameter aperture and was designed to hold the haptics of the IOL and to be adjusted to the front opening of the integrating sphere. The light source was connected with a UV-Vis optical fiber equipped with a microlens at the end to guide the light on the IOL surface. The signal is collected from another optical fiber is analyzed by the spectrometer and is processed by spectra suite software (Ocean Optics). Spectra were collected at ambient conditions and all the measurements were recorded twice and the spectra were averaged. First, the optical characteristics of the integrating sphere were measured. A dark transmission spectrum was recorded as background correction with the empty plastic custom insertand a light trap cover placed in the port of the sphere. A reference transmission spectrum was recorded by replacing the light trap with the spectraflect cover to ensure 100% transmittance. The transmission spectrum of each IOL was acquired over the spectrum range of 360 to 1100 nm but the visible-near infrared region from 420-900 nm was selected for notice to avoid the signal noise at the spectrum region close to the response of the spectrophotometer.
Results
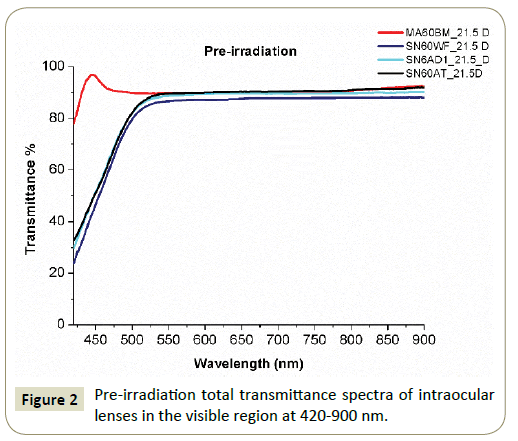
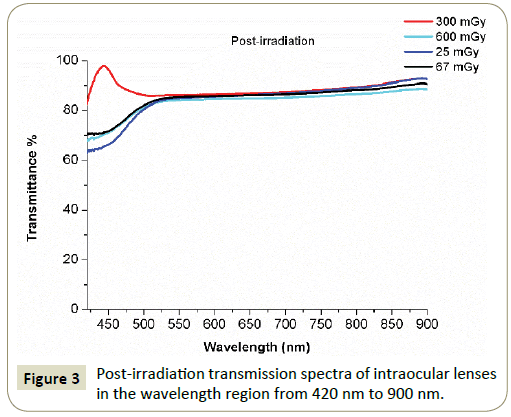
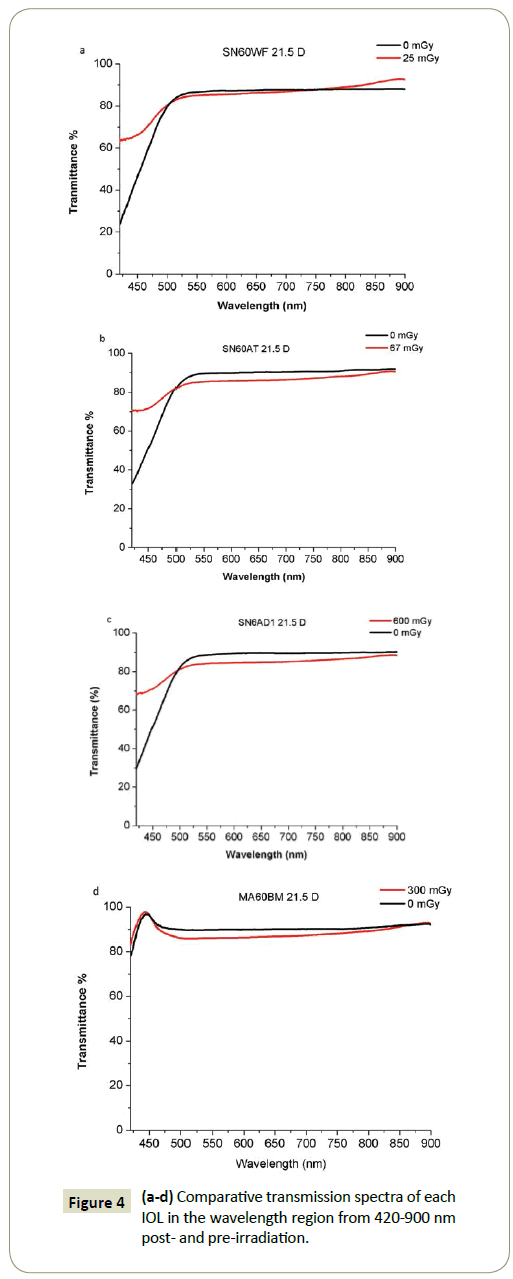
The pre-irradiation transmission spectra of all the IOL are presented in Figure 2, while Figure 3 shows the transmission spectra of the 3 yellow-azo dye IOLs (SN60WF, SN60AT and SN6AD1, Alcon) after irradiation to doses of 25 mGy, 67 mGy, 600 mGy and of the undoped hydrophobic IOL (MA60NM, Alcon) at dose of 300 mGy. Comparative transmission spectra from the IOLs pre-and postirradiation are presented separately in Figures 4a-4d.
The transmittance was precisely calculated according to the following relationship:
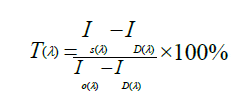
Where, Io is the reference light intensity passing through the empty plastic insert as it was recorded by the spectrophotometer. ID is the dark intensity recorded by the spectrometer with the light source blocked by the light trap. Isis the light intensity recorded when the light from the light source passes through the IOL which is placed in the plastic insert.
Discussion
According to the results, the transmittance of the 3 un-irradiated yellow azo-dye doped IOLs increases approximately linearly from ~25% to 30% up to ~80% as the wavelength increases in the shorter blue lightregion from 420-500 nm and reaches to a plateau of 87% to 90% approximately in the spectrum region from 550-900 nm (Figure 1). The undoped hydrophobic acrylic IOL shows a different behavior in the shorter wavelength region due to the absence of the yellow azo dye with the transmittance to obtaining the high value of 97%.
After the exposure to x-ray irradiation, the transmittance of the yellow azo-dye doped IOLs increases non-linearly in the blue light region from 420-500 nm showing a significant raise up to 60.5%- 70% at 420 nm. In the visible-near infrared spectrum range from 550-900 nm the transmittance of all the doped IOLs seems to be affectedslightly even at highest doses, while the undoped IOL appears almost unaffected in all the spectrum range.
Comparing the transmission spectra of each IOL pre and postirradiation, we observed that in the spectrum region from 420- 500 nm theIOLs show an increased transmittance Twith a highest ΔΤ changeequal to 35%, 37%, 38% at 420 nm for doses of 25 mGy, 67 mGy and 600 mGy respectively. In the residual visible region the transmittance is decreased by percentage 2%, 5% and 6% respectively. In the case of the undoped IOL, the transmittance retains almost the same value with a difference ΔΤequal to 4% from 500-900 nm.
These findings show that the yellow azo dye of the IOLs are affected by irradiation with x-rays as the irradiated IOLs present higher transmittance than the un-irradiated IOLs in the blue light region, while the undoped hydrophobic acrylic lens remain unaffected. This fact indicates that the yellow-azo dye doped IOLs lose the block-barrier against harmful UV radiation and short wavelength blue light after interaction with ionizing radiation. However, in the residual visible spectrum region the reduction of the transmittance of all the IOLs after x-ray irradiation is low. To correlate the changes on the transmittance with the opacification of the eye lens, the crystalline natural lens of a 53 and 75 years old person transmits only the 70% and 20% of the visible light respectively, in comparison with the 87-90% and the 84% to 86% which the implanted IOL transmits pre and post-irradiation, respectively [21].
Conclusion
The x-ray irradiation at clinical doses used in interventional radiology and cardiology procedures of human eye affects significant the filter protection of the intraocular lenses against the natural exposure to the damaging UV and short wavelength blue light, while the transmittance in the visible region is slightly reduced.
References
- https://www.uniteforsight.org/ global-health-university/cataract-surgery
- ICRP (2007) International Commission on Radiological Protection Recommendations of the International Commission on Radiological Protection. ICRP. Publication. 103: 1-7.
- ICRP (2012) ICRP statement on tissue reactions/early and late effects of radiation in normal tissues and organs – Threshold doses for tissue reactions in a radiation protection context. ICRP Publication 118. Ann. ICRP 41:1-322.
- Bolch WE, Dietze G, Petoussi-Henss N, Zankl M (2015) Dosimetric models of the eye and lens of the eye and their use in assessing dose coefficients for ocular exposures, Ann ICRP 44: 91-111.
- Broughton J, Cantone MC, Ginjaume M, Shah B (2013) Report of Task Group on the implications of the implementation of the ICRP recommendations for a revised dose limit to the lens of the eye. J Radiol Prot 33: 855–868.
- Efstathopoulos EP, Pantos I, Andreou M, Gkatzis A, Carinouet E, et al. (2011) Occupational radiation doses to the extremities and the eyes in interventional radiology and cardiology procedures. Br J Radiol84: 0-77.
- Efstathopoulos EP (2016) Occupational eye lens dose in interventional radiology and cardiology: New insights, Imaging Med. 8.
- Sankar V, Kumar TK, Punduranga KR (2004) Preparation, characterization and fabrication of intraocular lenses from photon initiated polymerized poly (methymethacrylate). Trends Biomater Artif Organs 17: 24-30.
- McLeod SD, Portney V, Ting A (2003) A dual optic accommodating foldable intraocular lens. Brit J Opthalmol 87: 1083-1085.
- Downes SM (2016) Ultraviolet or blue-filtering intraocular lenses: What is the evidence? Eye (Lond) 30: 215-21.
- Werner L (2007) Causes of intraocular lens opacification or discoloration. J Cataract Refract Surg 33: 713–726.
- Kocak N, Kaynak S, ILknuk T, Ozkan S, Erdogan G, et al. (2007) Effect of ultraviolet B radiation on the absorption characteristics of various intraocular lenses. Ophthalmologica 221: 29–35.
- https://www.who.int/blindness/causes/priority/en/index1.html
- Shore RE, Neriishi K, Nakashima E (2010) Epidemiological studies of cataract risk at low to moderate radiation doses: (Not) Seeing is believing. Radiation Research. 174: 889–894.
- Ellerin BE, Nisce LZ, Roberts CW, Thornell C, Sabbas A (2001) The effect of ionizing radiation of intraocular lenses. Int. J. Radiation Oncology Biol Phys 51: 184–208.
- Fontenla DP, Ahmad M, Chui CS, McCormick B, Abramson DH, et al. (1995) Effect of ocular implants of different materials on the dosimetry of external beam radiation therapy. Int J Radial OncolBiol Phys 32: 1477–1480.
- Moritake T, Matsumaru Y, Takigawa T, Nishizawa K, Matsumura A, et al. (2008) Dose measurement on both patients and operators during neurointerventional procedures using photoluminiscence glass dosimeters. AJNR Am J Neuroradiol 29: 1910–17.
- Sánchez RM, Vañó E, Fernández JM, Rosati S, López-Ibor L ( 2016) Radiation Doses in Patient Eye Lenses during Interventional Neuroradiology Procedures AJNR Am. J Neuroradiol 7: 402-407.
- Vanhaverea F, Carinoub E, Domienikc J, Donadilled L, Ginjaumee M, et al. (2011) Measurements of eye lens doses in interventional radiology and cardiology: Final results of the ORAMED project. Radiation Measurements 46: 1243-1247.
- Akinay A, Ong MD, Choi M, Karakelle M (2012) Measuring ultraviolet-visible light transmission of intraocular lenses: Double-beam mode versus integrating-sphere mode. J Biomed Opt 17: 105001-105007.
- Mainster MA, Sparrow JR (2003) How much blue light should an IOL transmit? Br J Ophthalmol. 87: 1523–1529.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences