Optimization of Pertubation Effects and Radiotherapy Facillities of the General Hospital of Douala; Staff, Equipment and Infrastructure
Tetchoka Manemo Cedric, Samba Ngano Odette, Alain Jerve Fotue, Towa Arnold Cedric and Lukong Cornelius Fai
Tetchoka Manemo Cedric*,Samba Ngano Odette*, Alain Jerve Fotue, Towa Arnold Alain Jerve Fotue, Towa Arnold
Department of Physics, Electronics and Signal Processing Research Unit, University of Dschang, Dschang, Cameroon
- *Corresponding Author:
- Tetchoka Manemo Cedric
Department of Physics, Electronics and Signal Processing Research Unit,
University of Dschang,
Dschang,
Cameroon,
Tel: 676394161;
E-mail: tetchoka2010@yahoo.com - Samba Ngano Odette
Department of Physics,
Electronics and Signal Processing Research Unit,
University of Dschang P.O. Box 67 Dschang,
Cameroon,
Tel: 675389140;
E-mail: nosambacm@yahoo.fr
Received Date: November 13, 2020; Accepted Date: November 30, 2020; Published Date: December 07, 2020
Citation: Cedric TM, Odette SN, Fotue AJ, Cedric TA, Fai LC (2020) Optimization of Pertubation Effects and Radiotherapy Facillities of the General Hospital of Douala; Staff, Equipment and Infrastructure, Insights Med Phys Vol: 5 No: 3: 14
Abstract
In order to evaluate radiotherapy facilities and perturbation effects hindering the well function of the therapy unit of the General Hospital of Douala, we decided to conduct a retrospective, qualitative, quantitative and comparative study of the essential elements of this service over a period of 30 years using questionnaires and data sheets. Epi info software was then used to simulate our data and analysis done. From this study, no General Hospital of Douala never reached the ideal normative score of 100% from its creation in 1987 until 2018. The indicator related to the staff had a normative score of 74.80%, equipment 55% and infrastructure 58%. The most represented specialty RTTs 33.33%, RN 25%, MP 12.50%. Regarding infrastructure, there is a complete absence of the physico-dosimetric planning room, no brachytherapy machines during the last 3 years. This situation of disruption significantly compromises the quality of care offered to patients in this service and will only be solved by the establishment and application of voluntary and more objective strategies by the administration of this hospital and the state bodies in charge of health. Strategies sufficient staff, qualified and equipment more recent or more adapted to the most recurrent types of cancer
Keywords
Radiotherapy; Staff; Equipment; Infrastructures; Perturbation effect
Introduction
The incidence of cancer is increasing, particularly because of the increase in life expectancy arising from worldwide improvements in standards of living. According to recent estimates of the International Agency for Research on Cancer (IARC) and World Health Organization (WHO), approximately ten million new cases of cancer are being detected per year world-wide with slightly more than half of the cases occurring in developing countries. The birth of radiotherapy pursues its ultimate goal over the years to deliver an optimal effective dose to the tumor volume while preserving at best the holy tissues refined to become an essential method in the treatment of cancers in the world. Some developed countries such as France, Germany and the United States offer quality radiotherapy services because of their permanent staffing, equipment and state-of-the-art infrastructure that contributes to effective cancer control despite the increasing incidence of the plague (lamented by GLOBOCAN (2012)); which is causing the increase in life expectancy of cancer patients in these countries after the diagnosis of the disease.
In Cameroon, it was not until 1987 that radiotherapy services were born in the general hospitals of Douala and Yaoundé. According to World Health Organization WHO (2014) and GLOBOCAN (2012), in Cameroon the most prevalent cancers are breast cancer and cervical cancer in women, while in men, prostate and lung cancer are the most common. More than 80% of cases are diagnosed at an advanced stage of the disease and most of them die within 12 months of diagnosis. These two radiotherapy departments have therefore done their best to cope with the growing rate of cancer despite local constraints such as: insufficient staff, infrastructure, equipment with aging appearance and recurrence of equipment failures due to the lack of an effective maintainer that interrupts the treatment of patients. This is how the number of patients treated per day becomes quite important at the HGD (whose wait is quite uncomfortable), making it difficult to take care of, treat and improve the living conditions of patients. It is estimated that approximately 3300 teletherapy machines are currently installed in developing countries. This figure is below the estimated needs of almost 5000 and about 15000 machines by the year 2020 [1]. Taking this into account and in addition to the great need for trained and qualified professionals (Radiation Oncologists (RO), Medical Physicists (MP), Radiotherapy Technicians (RTTs), Radiation Protection Officers (RPO), Dosimetrists (DM) and Maintenance Engineer (ME)), the future development of teletherapy infrastructures for cancer treatment appears to be a substantial undertaking.
In Cameroon, a developing country in centre Africa, there is actually one teletherapy machine and 4 Radiation Oncologists serving a population of 25 million, both of whom are based in the capital of Yaoundé and economic capital Douala. Efforts led by the Ministry of Health to subsidize generic chemotherapy and to screen for cancer have been seriously under-funded, so that many patients who are diagnosed with treatable cancers die unnecessarily. According to the Globocan estimate 2012, breast cancer is the most frequent cancer in women with an incidence of 35.25 per 100000 in Cameroon [2]. These multiple problems specific to Cameroon's RT services, coupled not only with the lack of an effective local strategy for cancer awareness and prevention, but also with the growing number of cancer cases, lead us to think of the need to evaluate improvements of radiotherapy facilities in the HGD, as well as to examine the perturbations that have caused or lead to its constraints.
The objective of this work is first to conduct a comparative study on the improvements of the radiotherapy department of the HGD in terms of: infrastructure, equipment and personnel with the requirements of international standards and thereafter identify the potential consequences (pertubation effects) as well as the current difficulties faced by the staff members of this service and finally try to propose solutions.
This study was aimed at presenting to the ministry of public health data or information which is very relevant in the improvement of radiotherapy facilities, knowing how good we are compared to the standards of IAEA, proposing recommendations regarding staff and equipment, to fight against increasing cancer incidence, help in the prevention of morbidity and mortality. The methodology and data analysis procedures used in this study were scientifically valid. During data collection, there was sufficient monitoring to remain scientific and maintain the quality of the data collected.
Materials and Methods
We carried out a retrospective cross sectional hospital based study at the GHD targeting administrative and technical staff of the radiotherapy unit alongside its infrastructure and equipment. Sampling was exhaustive involving those working in the therapy unit with at least 3 years or work experience and involved a total of 16 workers. Then, the questionnaire and informed consent form were developed using the software Epi Info version 7.2.2.6 the data collection tools were pretested and validated. All these were then submitted to the ethical committee of the department of physics of the University of Dschang for ethical evaluation and approval. Also, an administrative authorization was obtained from the GHD. Collection was done by a single interviewer. All eligible participants who were willing to participate were enrolled in the study. The major analyses involved included calculation of frequency and their confidence intervals at 95% (for qualitative variables such as the general characteristics of the participants or socio-demographic variables (age, sex, level of qualification or training, specialty, professional experience in the field of specialization) of the staff, the main the types of cancer treated at the GHD, the treatment methods employed, the essential equipment and the existing and operational staff, the evolution of the number of staff, the equipment and the infrastructures, the opinion and the problems encountered by staff in the radiotherapy department of the HGD. Another data sheet has been provided to the Deputy Head of Unit for retrospective analysis of personnel, equipment and infrastructure from the creation of the center until 2018.
Results and Discussion
Results for staff
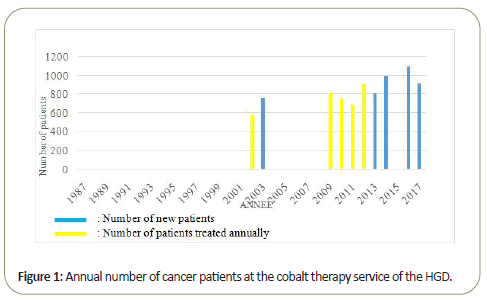
Specification of the radiotherapy service studied: Figure 1 represents newly diagnosed patients (blue band) and annual diagnosed patients (yellow band) at the GHD. The unit is made up of 16 members of whom; 4 did not contribute to our study because of their absence in the service throughout our stay at the GHD and finally 1 who did not respond favorably to our inclusion criteria. The therapy had no regular archives from its creation till 2001 and has an average number of 500 cancer cases annually.
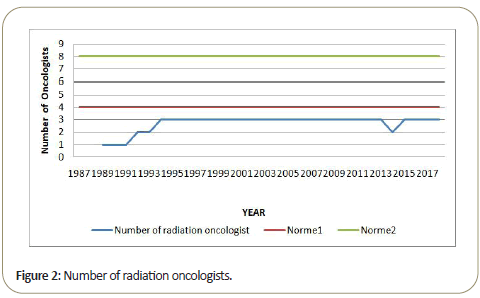
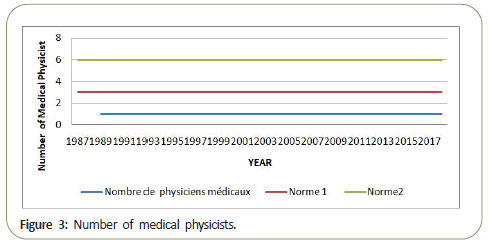
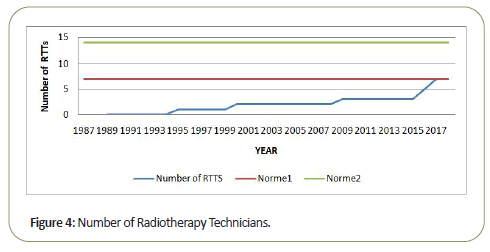
The curve in green indicates standard number of personnel for a centre having an annual number of 1000 patients as prescribed by the IAEA. Since the GHD receives an annual number of about 400 patients, we therefore derived another standard for a centre treating less than 500 patients per year which is indicated in red. The blue curve indicates the situation in GHD.
General characteristics of participants and overall knowledge vis a vis cancer and radiotherapy: From our analysis, most of the staff are male (62.50%) with predominance of RTTs (62.50%), RN(25%), MP(12,50%), almost similar to that obtained by Tetchoka et al. [3] at the GHY RTTs (42.50%), for a population of 10. Only 75% of the staff had undergone professional training with just 33.33% lasting for 4 years and above in their respective domains, the rest in-situ training with no skills. It was however amazing to notice that only 37.5% of the staff attend capacity building seminars probably due to lack of financial and technical resources that can allow inclusion to the training programs. Moreover, 87.5% constantly give monthly reports about radioprotection dosimetry to ensure safety. For people working with ionizing radiation in a medical setting, the maximum dose limit is 20 mSv per year [4], 60% of the staff benefit from rest days (3-8 per month) thereby giving them enough rest to enhance work effectiveness and output. Again 12.50% of perturbation effects were related to lack of capacity building seminars, 12.50% due to lack of Maintenance Engineers and 37.50% due to insufficient staffing.
Staff present or having existed in the radiotherapy department of the HGD: For a basic radiotherapy centre treating up to 1,000 patients a year with two megavoltage teletherapy machines, a high-dose rate brachytherapy unit and other standard equipment (a conventional or computed tomography simulator), immobilisation devices, shielding devices, a TPS and physical dosimetry tools; the IAEA recommends a staffing of around 20 (4-5 radiation oncologists, 3-4 medical physicists, 7 radiation therapy technologists, 3 radiotherapy nurses, and a Maintenance Engineer) [5]. In more detail, this team consists of a radiation oncologist-in-chief, one staff radiation oncologist per 200-250 patients, one radiation physicist for every 400, one dosimeters or physics assistant per 300 patients, one mould room technician per 600 patients, four RTTs (radiation therapy technologists) per megavoltage unit treating up to 50 patients per day, 2 RTTsimulation for every 500 patients simulated annually, and RTTbrachytherapy as needed, as well as a nurse for every 300 patients, a social worker, a dietician, a physiotherapist and a Maintenance Engineer or electronics technician [6]. The staff requirements will increase if special or advanced techniques such as threedimensional treatment planning or conformal radiotherapy are employed.
Radiation Oncologist (RO): From Figure 2, we see that the center began its activities in 1989 with a compliance rate of 25% relative to the specialty radiation oncologist (RO) until 1991. In 1992, this rate increases to 50% and then to 75% in 1994, then relapse in 2014 to 50% with the death of one of the radiotherapists who was replaced the following year (2015) by another; restoring the compliance rate to 75%, which will remain until 2018. Since the creation of this service at the HGD, the maximum number of radiation therapists is 3, well below the minimum of 4 recommended radiation therapists by the IAEA (2007). Following the death that occurred in the specialty in 2014, between 2013 and 2015 the work of the two ROs present had considerably increased because the number of patients by radiotherapy oncologist increased from 270 patients per RO in 2013 to 333 patients per RO in 2015; figures already well above the IAEA standard (2007) in 2013 and being 200 to 250 patients annually per RO. This overload situation has disrupted treatment by increasing not only the waiting time in consultation with patients but also the waiting time before care. It turns out that to compensate for disruptions in this specialty, additional recruitments must be made: it will for example recruit 1 RO to be in compliance with the standard 1 or 5 additional RO to be in compliance with the standard 2.
Medical Physicists (MP): From 1989 to 2018, Figure 3 shows that the center had a compliance rate of 33.33% for the specialty of medical physicist. Since the creation of the center, the position of medical physicist is held by one and only one person tending to retirement today. This reduced number of MP is similar to the maximum number of MP observed at the GHY [3] and it highlights the significant gap between the situation of the GHD (and Cameroon) for the specialty and the recommendation of the IAEA for the number of Medical Physicists (3 medical physicists) for a basic RT center. This insufficiency leads to a longer wait for dosimetric calculations for each patient, and prolongs the waiting time before patient care.
To overcome the disruption caused by this number of MPs, it is necessary for the HGD to acquire 2 additional MPs to be in compliance with the standard 1 as it was done in Senegal at the RT services [7].
Radiation Therapy Technicians (RTTs): According to Figure 4, the RT service at the GHD operated without a RTT from 1989 to 1994. In 1995, the rate increases to 14.28%, then to 28.57% in the year 2000, then 42.85% in 2009 before reaching the norm 1 in 2017. These multiple variations in the compliance rate for the specialty of RTTs allows to realize that before 2017, the handling of the treatment devices within the service was assured by the specialists of RT (RO and PM) between 1989 and 1994, something having a significant impact not only on the radioprotection of the personnel involved but also on the circuit of patient treatment by increasing the waiting time of the latter. Thus to solve these perturbation due to the insufficient number of RTTs although having considerably evolved until 2017, the GHD should equip itself with 7 additional RTTs in order to meet the norm 2 to be able to serve properly and efficiently the number of growing patients she has been responsible for in recent years.
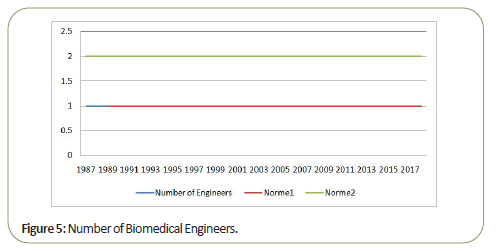
Biomedical Engineers (BE): In view of Figure 5, from 1989 to 2018, the HGD operates with 100% compliance with norm1 for the biomedical technician specialty. Several devices during their existence at the GHD were abandoned due to technical failures that he could not ensure the restoration or maintenance. Moreover these disturbances due to the incompetence of the biomedical technician in the RT service entails long interruptions in the treatments because of the uncorrected breakdowns. To compensate for this the HGD should contribute to the training of a biomedical technician specialized in RT service devices as recommended by the IAEA standards, for a better understanding of the technology as well as to ensure smooth logistics to obtain spare parts in case of failure where the need arises.
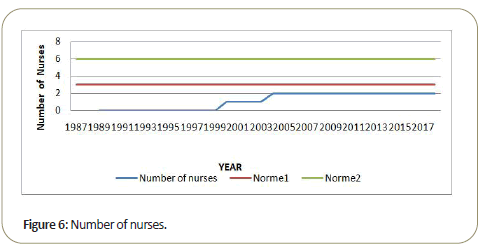
Radiotherapy Nurses (RN): From the opening of the service until 1999, the latter did not have any nurses (Figure 6). It was in the year 2000 that the compliance rate for this specialty became non-zero, rising to 33.33% then to 66.66% in 2004 and remained the same and lower than the norm 1 (3 RN) up to 2018. This last value is equivalent to the maximum rate obtained at the GHY in the same specialty [3]. This reduced number of nurses sometimes leads to frustrations in the service because with the large number of patients received daily, several tensions arises because of the feeling of rejection developed by some patients feeling misunderstood or misguided. Thus, these disruptions related to the insufficient number of nurses could be ended if the need for 4 additional nurses for the service is filled in order to reach the norm 2. Allowing the listening and a more efficient follow-up of each patient.
Results for equipment
The most common cancers in at GHD are cervical (35%), breast (25%), skin(15% mostly albinos), prostate(15%). This clearly shows that women make up the majority of patients treated by the main methods; surgery (27.27%), external beam therapy (27.27%), chemotherapy (36.36%) or more often a combination as advocated by [8]. Similar data were found in Paraguay by [9]. According to our analysis, the on-site radiotherapy equipment is essentially reduced to the EQUINOX 100 Cobalt teletherapy machine. The absence of equipment such as a brachytherapy pre-loader, a simulator, a TPS, QC equipment and mushroom causes considerable consequences disrupting not only the pre- established treatment procedure but also the treatment duration. Basically there is no chemotherapy machine. The most frequently encountered perturbation related to equipment are due to; absence of Maintenance Engineers, absence of QC of machines, lack of simulators and adequate 3D devices, insufficient nursing materials.
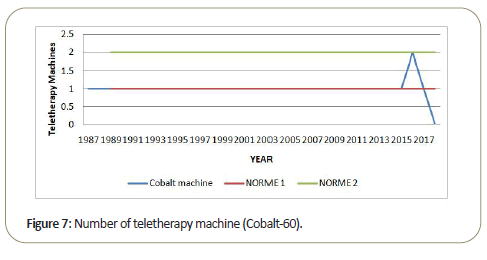
Megavoltage teletherapy unit: From 1989 to 2015 (Figure 7), the GHD RT service operates at 100% compliance with norm 1 in megavoltage teletherapy with a cobalt bomb (ALCYON II) for a number of patients approaching 1000 in 2014. In 2016, with the start-up of a second cobalt teletherapy machine (EQUNOX 100); this rate got to norm 2 before falling back to normative score 1 following an uncorrected ALCYON II failure in 2017, then becomes zero in 2018 following the technical failure of EQUNOX 100. Thus between the opening of the center and 2015 athough evolving under norm 1 in megavoltage teletherapy unit, the GHD has been confronted with a growing number of patients and difficulties due to the lack of maintenance of teletherapy devices.
This is more alarming from 2012 with the technical breakdown that affected the GHY's RT service. The GHD receives a large flow of patients. The GHD ALCYON II alone served a population of more than 20 million (if we ignore the number of patients from neighboring countries in Cameroon), which is well beyond the acceptable global standard of: 1 megavoltage machine for 120000- 250000 people proposed by [7]. Thus, if we refer to this additional standard, the national level shows the perturbation due to the insufficient number of RT machines per inhabitant, which in turn leads to the displacement of patients from remote regions, the financial cost in the quest for therapy, accommodation problems and languages etc. curbing the best care of patients.
Moreover, despite the fact that 2016 represents the only year in which the center reached normative score 2. As early as 2017, a series of technical breakdowns (that of Halcyon II and then EQUINOX 100) completely paralyzed the RT service in 2018. Failure coupled with the growing number of patients constitutes a significant disruption in the service. Indeed, these disturbances inevitably cause patients to increase the waiting time before the therapies, and an extraordinary use of RT devices in order to respect the treatment protocols established for each patient before the breakdowns.
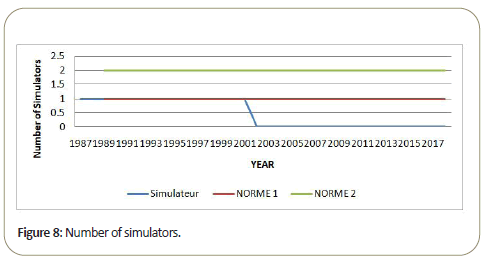
The simulator: From Figure 8, it can be seen that from 1989 to 2001, the center has a compliance rate equivalent to norm1 pertaining to simulation equipment (VERASIM). This rate becomes zero (and equivalent to that observed at the GHY [3]) from 2002 following an unrepaired failure of the simulator. This failure significantly affected the treatment circuit of patients and their radiation protection, representing a huge disruption. Consequently, the determination of the regions of the body to be treated and the organs to be protected was no longer optimally done. This disruption due to the absence of the simulator will push radiotherapists to perform manual simulations directly on the patient during the first irradiation session, using their knowledge of human anatomy and medicine. Thus, in order to make the treatment circuit proposed to patients more efficient, the GHD should equip itself with RT simulation equipment for which it will have to provide quality maintenance.
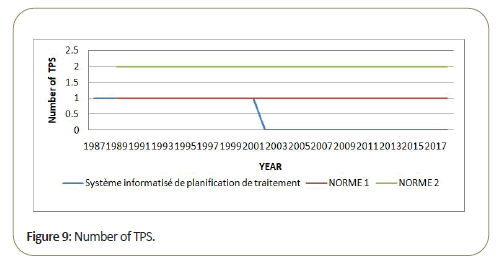
The treatment planning system: In Figure 9, from 1989 to 2001, the GHD operated with 100% compliance with norm 1 pertaining to the treatment planning system (Rokc's). In 2002, this rate becomes zero because of the unrepaired malfunction of the simulator that rendered the TPS that had been used until then unworkable. Thus, in 2002, the RT service of the HGD operates without TPS. This figure is well below the acceptable standard proposed by the IAEA, a detrimental situation that occurs in a period when the number of patients has increased over the years. The service disruption caused by the impossibility of using the TPS has had a significant impact on the treatment provided to patients because it is now a little more complicated to optimally determine the dosimetric parameters, by manual calculation, for the treatment of each patient and therefore difficult to achieve a more optimal treatment of diseases. Hence there is a need for the HGD to have a TPS.
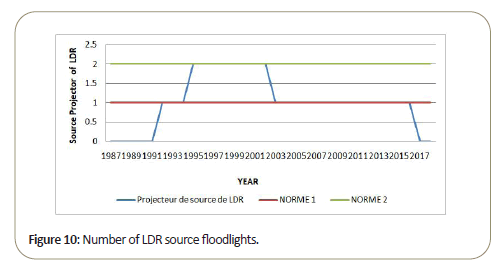
Brachytherapy unit: From Figure 10, from 1989 to 1991, the GHD RT service had no brachytherapy equipment, including the LDR source projector. Between 1992 and 1994, it operated under a 100% compliance rate of norm 1 by acquiring its first LDR source projector (CERVIFIX) and then evolves at a 100% compliance rate of norm 2 between 1995 and 2002 with a second LDR source projector (AMRA, cesium 137). The compliance rate of the number of LDR source headlamps dropped to 100% of norm 1 in 2003 and remained there until 2016 before becoming zero again in 2017. Thus between 1995 and 2002 brachytherapy treatments were at their peak with the simultaneous presence in the service of two LDR source projectors for a fairly bearable number of patients as recommended by the IAEA. From 1989 to 1991, the lack of a brachytherapy machine was probably due to the embryonic state of the department, which had first to analyze the demand, a response to demand confirmed by the equipment endowments LDR between 1992 and 1995. The same non-existence of brachytherapy machines was found in several African countries such as Congo, Uganda and Liberia by F.A Durosinmi-Etti (1991), showing their delay in terms of brachytherapy at African countries such as Egypt, Senegal and Kenya were already offering brachytherapy care. This situation worsened considerably after 2016 due to the same causes leading to the lack of LDR brachytherapy equipment (which in many ways was not well suited to the situation) within the HGD's RT service. These pertubations are probably due to uncorrected breakdowns of brachytherapy equipment and/or non-renewal of the equipment concerned. Thus in order to respond appropriately to the growing demand for care for cancer cases such as cervical cancer, the HGD should have a brachytherapy service that is more suitable and why not more modern.
Noncommercial and/or non-functional equipment of the GHD: Since the creation of the RT service until 2018, some essential equipment for treating patients and making recommendations from the IAEA are missing from the technical platform. This goes a long way to contribute to the malfunctioning of the unit and increase perturbation effects. Such equipment includes:
An orthovoltage unit: more suitable in the treatment of superficial tumors;
A device for immobilizing the patient: to avoid the risk of irradiation of healthy tissue due to involuntary movements or not of the patient;
Beam measuring equipment+quality control and radiation protection equipment: useful for ensuring the integrity of the equipment, ensuring the quality of the equipment and the treatment provided;
An X-ray C-arm for verification;
A complete range of applicators: necessary to better focus the irradiation beams and to apply the prescribed doses optimally;
Physical quality control equipment; despite the fact that these controls, although effective are carried out by institutions outside the GHD's RT service.
Results for infrastructure
The bunker has megavoltage: Since the opening of the center, it has always operated with a compliance rate of 100% to norm 2 for megavoltage bunker (Figure 11). This rate is largely in line with the IAEA recommendation and clearly addresses the number of patients treated at the GHD in recent years.
The center has always had a 100% compliance rate with norm 1 for the simulator room (Figure 12). This rate is in line with the IAEA recommendation. However, the failure of the VERASIM simulator in 2002 significantly affected the operation of the GHD simulator room. This is why, due to the lack of equipment in this room, it has been converted by the staff into classroom and meeting room. It is clear that in order to provide the best quality care, the GHD should equip this room with the device for which it was reserved.
The mold room: The GHD RT service has always had a 100% compliance rate with norm 1 for the mold room (Figure 13). This rate is in line with the IAEA recommendation. However, it should be noted that as soon as the center was opened the CEROBEN Polystyrene and Casting Shop installed in this room was never used due to the lack of CEROBEN alloy. This absence hindered treatment sessions: patients have never owned a personalized cache, which no doubt increases the risk of risky organ irradiation or nearby healthy tissue to tumor masses; making the treatments less optimal. To mitigate this disruption in service, the HGD should either supply this alloy or procure a new, more modern personalized cache maker.
The clinical space: Since 1989, the center has a 100% compliance rate with norm 1 for clinical space (Figure 14). This clinical space is in accordance with the IAEA recommendation. It has a fairly large clinical area including: examination rooms, doctors' offices, a physicist's office, waiting rooms (invalid and invalid patients) having been enlarged in 2017, undressing rooms and a secretariat.
Infrastructure absent and/or unused at the HGD: Since the creation of the RT service, certain infrastructures essential to the service and recommendations from the IAEA are absent from the technical platform, Absences constituting additional pertubations due to the impossibility of using each of their functionalities. These include:
An X-ray bunker: to contain the orthovoltage unit;
An HDR or LDR bunker: to distribute brachytherapy care;
A dark room for the development of films;
A physico-dosimetric planning room: more suitable for a multidisciplinary discussion leading to the planning of the treatment of each patient (irradiation field, dosimetric parameters and fraction number, etc.).
In addition, some rooms have not been used for years in the service of RT GHD, thus disrupts the therapeutic habits of this service that until then contributed to better patient care. These include:
The simulator room, unused since the simulator crash occurred in 2002;
The mold room not used since the opening of the center due to the lack of CEROBEN alloy. Just before the start in 2017 of the renovation works of the General Hospital of Douala planned by the three-year emergency plan (PLANUT), the service was quite uncomfortable for the staff but especially for patients who have been forced to take refuge in the service; something that makes waiting for patients a bit more tiring. These renovations will significantly improve the daily comfort of staff and patients, but it is not possible to do so with GHD's RT service infrastructure as it was done at the HGY in 2016 with the construction of new bunker [3]. These renovations consist of expanding the space for the patient, the addition of air conditioning to the room and the room temperature. Therefore, this service will never reach the normative score in terms of infrastructure if nothing is done in that sense.
A little more daring than the PLANUT, the PIP 2015-2017 (public investment program), initiated by the Beninese government, aimed at making Benin an ideal cancer treatment centre in West Africa to be launched in April 2015 with the construction of a reference center in radiotherapy. Through three essential infrastructural components, namely the construction and equipment of a radiotherapy unit, a nuclear medicine unit and a complete pathology-anatomy unit, this center has been constituted as a single pole of excellence in its sub region, but for reasons specific to the sub-Saharan African economic context, work was interrupted at an embryonic stage two years later [10]. This shows the willingness of some African countries to aspire for quality services despite the perpetual brake of the economic context.
Conclusion
Evolving nowadays in a precarious context and limited resources, it is almost by abuse that the General Hospital of Douala holds the name of center of excellence if one refers mainly to its radiotherapy service, well that it serves cancer patients from its territory as well as some patients from its neighboring countries in the Central Africa sub region. This study was designed to assess the level of radiation therapy facilities at the GHD to determine whether it will be able to cope with one of the challenges of the century, namely the growing number of new cases of Cancer. Thus, it was a question of evaluating the evolution of the radiotherapy department of the GHD according to the elements: equipment, personnel and infrastructure of its creation until 2018 and afterwards to compare the data obtained in the first approach to the standards proposed by the IAEA in the case of a "basic" RT service, operating in an environment of limited resources. From our results it is clear that:
This center has never achieved the overall normative score of 100% from 1989 to 2018 for equipment, personnel and infrastructure.
The number of staff, although having evolved significantly since the creation of the center, is insufficient to support just half the number of patients it has actually received since 2016.
The equipment of the radiotherapy department of the GHD, although it may be considered obsolete in our time, has gradually been the victim of a large technical breakdown which, due to a lack of effective maintenance, rendered the service incapable of fulfilling its mission properly.
The facilities that make up the HGD's RT center have never undergone any improvement in terms of room or space. This has contributed to the burden on the staff and the longer waiting time for service of patients.
Overall, these multiple insufficiencies of the center are in themselves disruptions within the service because they slow or prevent the service from contributing to an efficient and optimal care of all the patients for whom it is responsible.
The cancer mortality rate will continue to increase if:
Existing centers do not receive strong grants and/or partnerships with centers of excellence in developed countries to facilitate the training of its staff in new cancer therapy techniques and procedures before providing them with more advanced equipment sophisticated than those currently present and better adapted to the types of recurrent cancers in Cameroon.
New radiotherapy center is not created with more vigor and objectivity.
Efficient prevention strategies, early diagnosis of the disease are not developed and implemented in all regions of the country.
If nothing is done properly, the situations will only get worse not only for the patients but also for the small staff who work with equipment that is not well adapted to a demand of care becoming more and more unmanageable. In such a context what about the future of cancer patients followed in the radiotherapy department of the GHD?
References
- International Atomic Energy Agency (IAEA) (2008) setting up a radiotherapy program: Clinical, medical physics, radiation protection and safety aspect, IAEA, Vienna.
- Sando Z, Fouelifack YF, Fouogue TJ, Fouedjio JH, Essame-Oyono JL (2015) Trends in breast cancer and cervical cancer incidence in Cameroon (central Africa) from 2004-2011. African J Cancer 7: 118-121.
- Cédric TM (2017) Improvement of radiotherapy facilities in Cameroon : Equipement and staffing. How good are we ? J Rad Res App Sci 12: 166-176.
- Cordoliani YS, Aubert B (2003) Exposition aux rayonnements ionisants des personnels médicaux Pour une catégorisation et une surveillance dosimétrique rationnelles. Radioprot 38: 483-491.
- Campbell OB, Arowojolu AO, Akinlade BI, Adenipekun A, Babarinsa IA (2000) Advanced cervical carcinoma in Ibadan, Nigeria: an appraisal of radiation therapy. J Obstet Gynecol 20: 624-627.
- Abdel-Wahab MM, Rosenblatt E, Pynda Y, Iżewska J, Zubizarreta E, et al. (2013) Status of radiotherapy resources in Africa: an International Atomic Energy Agency analysis. Lancet Oncol 14: e168-175.
- Brandon J, Daugherty LC, Einck JP, Suneja G, Shah MM, et al. (2014) Radiation Oncology in Africa: Improving Access to Cancer Care on the African Continent. J Rad Oncol 89: 458-461.
- Chuang LT, Temin S, Berek JS (2016) Management and Care of women with Invasive Cervical Cancer: American Society of Clinical Oncology Resource-Stratified Clinical Practice Guideline. J Oncol Pract 12: 693-696.
- G. Jacobson (2018) Improving quality of care and timely access to radiation therapy for patients with invasive cervical cancer at the National Cancer Institute Paraguay. Gynecol Oncol Rep 25: 82-86.
- Afangbedji G (2015) Infrastructures sanitaires: Les travaux d’un centre de radiothérapie lances. Quotidien La Nation.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences